Project Questionnaire for the Public and Patient Engagement Evaluation Tool
KEY FEATURES
COMMUNITY/ GEOGRAPHY
Community advisory councils, patients, family members, citizens
Health system staff
Patient partner representatives Health system organizations
Ontario, Canada
COMMUNITY ENGAGEMENT OUTCOMES
Strengthened partnerships + alliances
Broad alignment
Diversity + inclusivity
Partnerships + opportunities
Acknowledgment, visibility, recognition
Sustained relationships
Trust
Shared power
Structural supports for community engagement
Expanded knowledge
Broad alignment
Improved health + health care programs + policies
Broad alignment
PLACE(S) OF INSTRUMENT USE
Community/community-based organization
Hospital, clinic, or health system
LANGUAGE TRANSLATIONS
Dutch (unavailable publicly)
French
German (unavailable publicly)
Italian (unavailable publicly)
PSYCHOMETRIC PROPERTIES
Content validity
YEAR OF USE
2018
2012-2014
Assessment Instrument Overview
The Project Questionnaire for the Public and Patient Engagement Evaluation Tool (PPEET)1-4 has 28 questions for use by managers and sponsors of health system engagement activities. It assesses the quality and impacts of engagement. The Project Questionnaire is part of a set of three instruments that also includes the Participant Questionnaire and Organization Questionnaire for the PPEET.
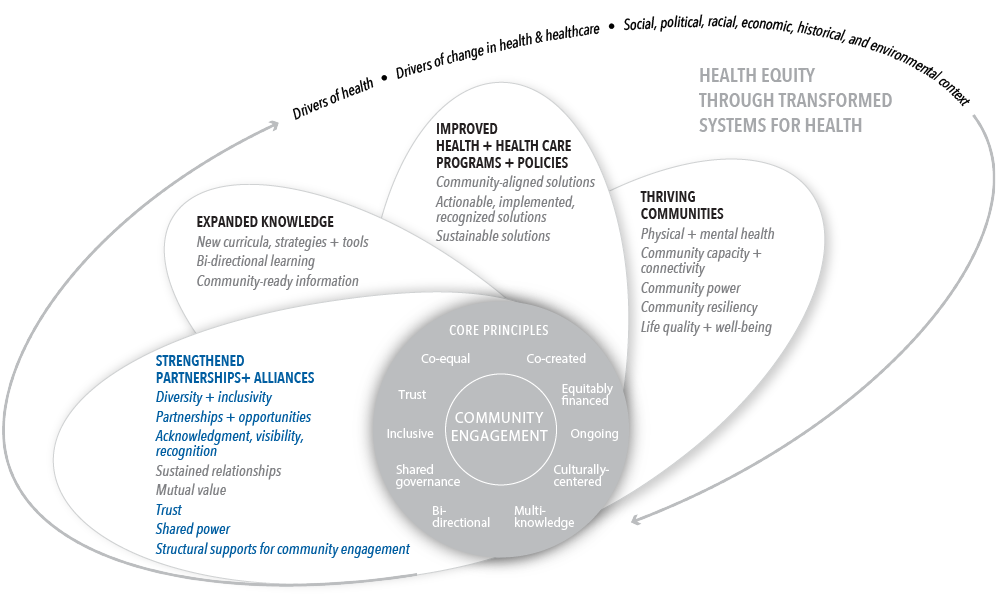
Alignment with Assessing Meaningful Community Engagement Conceptual Model
The questions in the Project Questionnaire for the PPEET were aligned to the Assessing Community Engagement Conceptual Model. Figure 1 displays the alignment of the Project Questionnaire for the PPEET with the Conceptual Model domain(s) and indicator(s). Where an instrument is mapped broadly with a domain or with a specific indicator, the figure shows the alignment in blue font.
Table 1 displays the alignment of the Project Questionnaire for the PPEET’s individual questions with the Conceptual Model domain(s) and indicator(s). The table shows, from left to right, the aligned Conceptual Model domain(s) and indicator(s) and the individual questions from the Project Questionnaire for the PPEET’s transcribed as they appear in the instrument (with minor formatting changes for clarity).
| CONCEPTUAL MODEL DOMAIN(S) AND INDICATOR(S) | ASSESSMENT INSTRUMENT QUESTIONS |
| STRENGTHENED PARTNERSHIPS + ALLIANCES; Broad alignment with all indicators in this domain | Overall, I was satisfied with this public and patient engagement activity. This public and patient engagement activity was a good use of our program resources. The output from this public and patient engagement activity enhanced decision making in this area.* Adequate time was allocated to plan and implement the public and patient engagement activity. |
| STRENGTHENED PARTNERSHIPS + ALLIANCES; Diversity + inclusivity | The project plan had a clear strategy to
Those most affected by the decision were appropriately represented in the engagement activity. |
STRENGTHENED PARTNERSHIPS + ALLIANCES; Partnerships + opportunities | As a result of our involvement in this initiative, our organization has a greater intention to collaborate with other organizations in the future. I would like to participate in public and patient engagement training to build my capacity to do more of this work. I will be more comfortable leading a public and patient engagement activity in the future. |
STRENGTHENED PARTNERSHIPS + ALLIANCES; Acknowledgment, visibility, recognition | Members of the organization’s leadership considered the public and patient engagement input. |
STRENGTHENED PARTNERSHIPS + ALLIANCES; Sustained relationships | All communications with participants throughout the engagement activity were well executed. Please list the names of the organizations that you collaborated with during the engagement activity and what plans, if any, you have for future collaborations with these organizations. |
| STRENGTHENED PARTNERSHIPS + ALLIANCES; Trust | The project plan
Please describe how the participant input summary report that was prepared was used and shared with participants. If no summary report was prepared, is there a plan to do so? If not, explain why. As a result of our involvement in this initiative, our organization has developed a greater trust in other organizations. |
| STRENGTHENED PARTNERSHIPS + ALLIANCES; Shared power | Members of the organization’s leadership used the public and patient engagement input to influence decisions related to healthcare improvement. Please describe how and at what stages the public and patient engagement input was considered in organizational decisions (list relevant sources of evidence for your response). If the input was not considered, explain why you think this was the case. We were able to identify shared goals with other organizations through the public and patient engagement activity initiated. We were able to achieve these shared goals through the public and patient engagement activity. |
STRENGTHENED PARTNERSHIPS + ALLIANCES; Structural supports for community engagement | The project plan included clear documentation of how the financial, logistical, and informational needs of participants (e.g., travel, dietary, interpretive, childcare, etc) would be accommodated. |
EXPANDED KNOWLEDGE; Broad alignment with all indicators in this domain | The output from this public and patient engagement activity enhanced decision making in this area.* |
IMPROVED HEALTH + HEALTH CARE PROGRAMS + POLICIES; Broad alignment with all indicators in this domain | The output from this public and patient engagement activity enhanced decision making in this area.* |
*Note that these questions are duplicated to reflect their alignment with multiple domains and/or indicators in the Conceptual Model.
Table 1 | Project Questionnaire for the Public and Patient Engagement Evaluation Tool questions and alignment with the domain(s) and indicator(s) of the Assessing Community Engagement Conceptual Model
ASSESSMENT INSTRUMENT BACKGROUND
Context of instrument development/use
The articles highlight the importance of public and patient engagement (PPE) in quality improvement efforts and that evaluating PPE often requires a balance between “relevance to practitioner needs” and “application of rigorous methods.”4 The articles discuss the development of PPEET, which leverages a 3-year collaboration between Canadian researchers and practitioners.1,4 PPEET “was launched as a simple-to-administer tool intended for use by a wide range of health system organizations to assess the quality and impacts of engagement, with the goal of contributing to both the practice and the science of public and patient engagement.”1 PPEET consists of three questionnaires to evaluate public and patient engagement: the Project Questionnaire (described here), the Organization Questionnaire (described in another assessment instrument summary), and the Participant Questionnaire (described in another assessment instrument summary).
Instrument description/purpose
The Project Questionnaire of the PPEET allows for capturing insights from those responsible for “planning, execution or sponsoring of engagement activities within organizations.”1 The instrument is for engagement practitioners and users, such as directors and managers of organizations or sponsors. The Project Questionnaire assess three areas:
- Integrity of design and process
- Influence and impact
- Collaboration and common purpose
The Project Questionnaire contains 28 questions that use a combination of open-ended, yes/no/don’t know, and five-point Likert scale responses. The Likert scale ranges from “strongly agree” to “strongly disagree.”4
The guidance for administering the instruments and the English and the French translations for the three questionnaires in the PPEET, including the Participant Questionnaire, can be accessed here: https://ppe.mcmaster.ca/resources/public-and-patient-engagement-evaluation-tool/. Please contact [email protected] to request the other language translations.
Engagement involved in developing, implementing, or evaluating the assessment instrument
“A pan-Canadian partnership of PPE practitioners and researchers” with the shared goal of developing a common evaluation tool formed through two consecutive research grants from the Canadian Institutes of Health Research. This research–practice collaborative “included representation from seven provinces, six regional health authorities and two provincial and local health organizations.”4
The development of the tool took place over a 3-year period. After a review of the literature, collaborative members engaged using structured e-mail, telephone, and face-to-face exchanges at workshops. A process with iterative rounds of review, also known as a modified Delphi process, was also used to review and prioritize insights. These activities contributed to the “identification of a set of overarching principles for carrying out high quality PPE activities that would serve as the foundation for the evaluation tool.” The workshops used break-out sessions and reporting back to the larger group, as well as larger group discussions, to identify and agree on a core set of outcomes. The core principles were mapped to outcomes and prioritized for inclusion in the tool. After developing “three discrete evaluation questionnaires for three different respondent groups,” the collaborative “tested the usability of the questionnaires preceding final revisions to the tool.”4
Patients and members of the public were only directly involved in the usability-testing phase. Participants, project managers and senior organizational personnel in two health regions tested the usability of the questionnaires.4 The tool underwent “additional feasibility testing in seven health system organizations in Ontario in collaboration with staff and patient partner representatives from each organization.” The PPEET was modified based on the results and the revised instruments, which launched in August 2018, were tailored to the specific respondent groups, had separate modules for different types and stages of engagement “(e.g., one time versus ongoing and planning versus implementation),” and included an increased balance in response options with opportunities for more in-depth follow up.1
Additional information on populations engaged in instrument use
Usability testing for the questionnaires took place with practice partners from two health regions and provinces. The Project Questionnaire “was distributed to 28 directors and managers across both organizations with 14 responses received.”4
Notes
- Potential limitations: The authors suggest that the focus throughout the process of developing the tool was on user needs (i.e., usability) rather than on psychometric properties, which may have led to a less robust evaluation tool. Since the tool development process was influenced by having short and easy to administer questionnaires, this may have “compromised the tool’s validity (e.g., number and specificity of statements used to assess a particular domain of practice, use of a 5-point vs. a 7-point scale).” Additionally, patient and citizen perspectives were not directly included in the development process for the PPEET beyond the usability testing phase. The PPEET’s focus on the health care context of Canada may limit its generalizability and applicability to “non-Canadian settings and to health-care organizations that focus on smaller and more specialized populations;” however, the extensive international literature review and participating partner organizations from major urban and regional referral centers that informed the tool included large and highly diverse populations.4
- Important findings: The authors indicate that to their knowledge, “this is the first collaboration of researchers and practitioners in the co-design of a comprehensive evaluation tool aimed at assessing the quality and impact of episodic and on-going PPE activities in health system organizations from three distinct perspectives – public and patient participants, sponsors and managers of PPE projects and organizational leaders responsible for PPE.” The tool strikes a balance between “the application of rigorous methods and relevance to practitioner needs,” Based on usability testing results, revisions were made to the Project Questionnaire to improve accessibility (e.g., clarity, layout).4
- Future research needed: Additional research and testing of the questionnaires is needed to understand if any weaknesses exist in the PPEET’s validity. Further testing is also needed on the feasibility of applying the tool to every type, level, and degree of PPE.4
- Supplemental information: The modified version of the PPEET, including the Project Questionnaire, released in 2018, can be accessed here: https://healthsci.mcmaster.ca/docs/librariesprovider61/default-document-library/ppeet-complete-set-final.pdf?sfvrsn=d1617fe6_2. Additional information on other settings this assessment instrument has been used in (i.e., emergency settings), populations in which the instrument has been tested (i.e., children with developmental delays, women with heart diseases) and modifications made can be found in the following articles:
- Ogourtsova, T., M. E. O’Donnell, J. H. Filliter, K. Wittmeier, Bright Coaching Group, and A. Majnemer. 2021. Patient engagement in an online coaching intervention for parents of children with suspected developmental delays. Developmental Medicine & Child Neurology 63 (6):668-674. https://doi.org/10.1111/dmcn.14810.
- Teed, M., J. Ianiro, C. Culhane, J. Monaghan, J. Takacs, G. Arthur, and A. Nash. 2021. Engaging Women With Lived Experience: A Novel Cross- Canada Approach. Journal of Patient Experience 8:1-7. https://doi.org/10.1177/23743735211008300.
- Bhati, D. K., M. Fitzgerald, C. Kendall, and S. Dahrouge. 2020. Patients’ engagement in primary care research: a case study in a Canadian context. Research Involvement and Engagement 6:1-12. https://doi.org/10.1186/s40900-020-00238-x.
- Drebit, S., K. Eggers, C. Archibald, R. Abu-Laban, K. Ho, A. Khazei, R. Lindstrom, J. Marsden, E. Martin, and J. Christenson. 2020. Evaluation of Patient Engagement in a Clinical Emergency Care Network: Findings From the BC Emergency Medicine Network. Journal of Patient Experience 7(6):937-940. https://doi.org/10.1177/2374373520925721.
- Thompson, A. P., S. E. MacDonald, E. Wine, and S. D. Scott. 2020. An Evaluation of Parents’ Experiences of Patient Engagement in Research to Develop a Digital Knowledge Translation Tool: Protocol for a Multi-Method Study. JMIR Research Protocols 9(8). https://doi.org/10.2196/19108.
We want to hear from you!
Assessing community engagement involves the participation of many stakeholders. Click here to share feedback on these resources, or email [email protected] and include “measure engagement” in the subject line to learn more about the NAM’s Assessing Community Engagement project.
Related Products