 Category: Diagnostic Imaging Devices
Category: Diagnostic Imaging Devices
Radiology relies on large resource-intensive equipment, such as computerized tomography (CT) scanners. Existing research has found that pathology and radiology services can be responsible for nearly a tenth of all health care system emissions. Scanning equipment has large electrical power requirements and their operation has been a focus of energy efficiency efforts on the part of manufacturers and hospitals, but other contributors to the carbon footprint of imaging are less well-known.
This brief summarizes a carbon footprinting study of a radiology department in the southeastern US with over 10 years of operation to identify typical hotspots and potential interventions to decrease product emissions. In the study, CT scanners were assumed to have a lifetime of 10 years, and their end-of-life treatment and disposal were not included.
Carbon Emissions Across Life Cycle
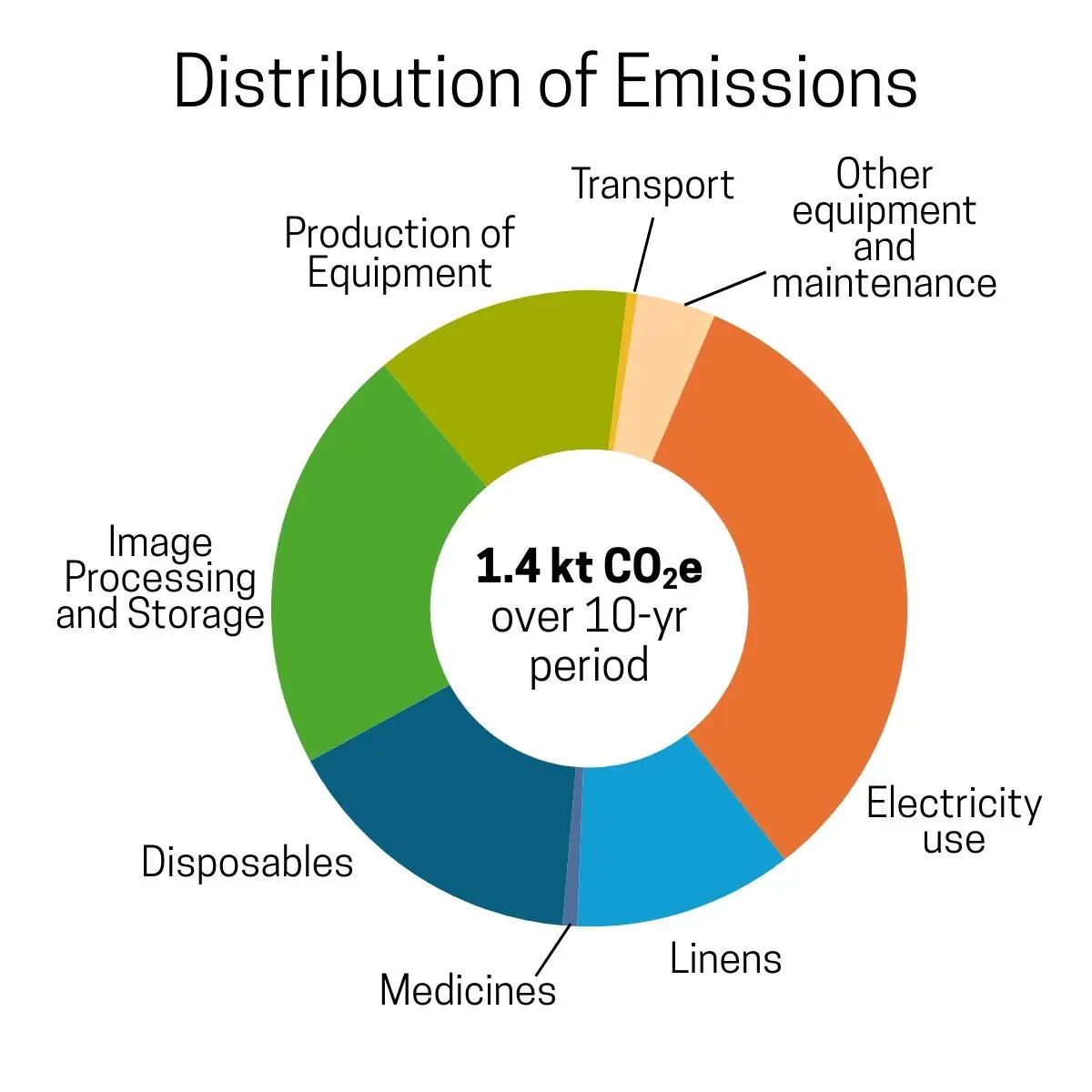
The major hotspot for CT scanners is electricity use during operation, followed by image processing and storage, disposable medical supplies, and production of imaging equipment. Production and laundering of linens worn by patients during scanning contributes more than 10% of the overall carbon footprint. The production of contrast agents and transportation of equipment make small contributions.
CT scanners operate within an ecosystem of other related equipment, supplies, and digital infrastructure. Looking at CT scanners in isolation, their production, transport, maintenance, and electricity use contribute to less than half of its total carbon emissions.
Focusing on Carbon Hotspots
The most impactful interventions focus on reducing emissions from electricity use; however, the presence of several additional, substantial contributors means that there is a diverse range of decarbonization opportunities. Based on these results, specific suggestions for different stakeholders include:
1. Avoid unnecessary usage:
⛨ Reduce overuse of disposable supplies and allow for patients to wear existing hospital linens.
⛨ Consider alternative diagnostic tests or smaller, portable units when full CT scans are not required.
2. Prolong equipment lifetime:
☑ Maintain scanners past the assumed 10-year lifetime to decrease per-scan emissions.
3. Reduce electricity use:
⚙ Procure renewable electricity (influencing both scanning and image processing and storage).
$ Select energy efficient scanners that allow for low-power idling or powering down when not in use.
Audience Key: ⛨ Clinicians | ☑ Administration | ⚙ Manufacturers | $ Procurement | ⛑ Regulators
Reference: Thiel et al. 2025. “Environmental Life Cycle Assessment of a U.S. Hospital-based Radiology Practice.” Radiology 13, no. 2: e240398.
Related Products

