Charles Bruner
Mercedes Samudio
Maria Schweer-Collins
Julie McCrae
Katherine A. Hails
Margaret Kuklinski
Lawrence S. Wissow
Marian F. Earls
JD Smith
Cady Berkel
Nikki Shearman
Joyce Javier
Katharine T. Hemady
Dani Dumitriu
Tyson Barker
Christina Bethell
Charles Bruner
Michele Polfuss
Overview
The health care field’s transformational shift toward value-based care is marked by significant efforts to create a higher quality, more equitable health care system. This includes (1) paying greater attention to health-related social needs and social determinants of health, (2) building a more robust public and community health system in poor and medically underserved communities, and (3) doing so with an emphasis upon racial equity as an underlying goal. While simultaneously improving the “triple aim” of health quality, advancing population health, and containing health care costs, much of the attention has been directed to adult populations. However, to improve population health, rectify health inequities, strengthen community health system responses, and secure high value from health investments, the evidence is clear that a major focus must be placed on children, and not solely on short-term cost containment.
The Collaborative on Healthy Parenting in Primary Care (HPPC) advances the work of the National Academies Forum for Children’s Well- Being through a focus on one particularly promising avenue for interventions. There is a wealth of evidence documenting the power of family- focused prevention programs to promote the physical and behavioral health and emotional well- being of children from before their birth through adolescence. These programs, several of which are described in greater detail in subsequent sections, range from strengths-based parenting and family- focused education and engagement programs in the primary care setting, culturally-tailored home visit interventions, and innovations focused on whole child and relational health, to programs that emphasize addressing the social drivers of health through screening and close-the-loop referrals for families connected to community resources. The majority of children (between 75 percent and 90 percent) attend a well-child visit each year (CDC, 2020). Primary care settings are thus an essential space for engaging with parents and children. Based on several recent convenings and discussions, including with the chairs of the Children’s Well- Being Forum and members of the Forum’s HPPC Collaborative, it has become evident that, while there is a growing number of equity-centered HPPC interventions, programs, and policies underway, to the authors’ knowledge, a synthesis of these efforts does not exist. Moreover, the current siloed, fragmented approach to primary care health systems and the health care workforce supporting parents and their children is unsustainable and operating with leaner resources; this is particularly true for entities, such as federally qualified health centers (FQHCs) that serve medically underserved youth and families. The urgency for this synthesis is reaffirmed by the recently released Surgeon General’s Advisory on the Mental Health & Well- Being of Parents, which brings attention to the high level of parental stressors that can impact mental health and well-being and explicitly calls for increased investments, implementation, and research on HPPC interventions to better support parents (Office of the Surgeon General, 2024).
This discussion paper seeks to advance the field by taking a critical look at existing efforts to advance HPPC and suggesting next steps to move the field toward additional innovation, diffusion, scaling, and adaptation of effective interventions. The authors recognize that, while there is a strong evidence base for existing HPPC interventions that work, there are also interventions with great potential currently being implemented in the field for which more research and documentation is needed. Thus, this paper seeks to shed light on both established and promising interventions. Section 1 describes the literature on parent engagement in HPPC program and practice design, implementation, and evaluation, with an emphasis on parents from marginalized backgrounds or limited opportunity settings and how to ensure they are part of the child’s health transformation process. Section 2 provides an overview of innovative and promising HPPC interventions that demonstrate implementation feasibility to strengthen the pediatric primary care system and workforce capacity to promote effective parenting. Section 3 discusses the key elements contributing to effective scaling and sustaining of HPPC interventions. The fourth and concluding section discusses core policy levers, with a particular focus on the role of federal policy and funding to advance HPPC interventions as a means of advancing health equity.
Methodology and Guiding Frameworks
This work reflects a multistakeholder, inter- disciplinary approach through several mechanisms. First, an open request for information (RFI) through the National Academies was released in January 2024, soliciting the input of a wide variety of stakeholders in the aforementioned areas of interests, including clinicians, researchers, parents and families, policymakers, and the general public. Second, the authors conducted an assessment of the current state of the evidence of HPPC interventions, including a review of eight previously identified reports (each with its own methodology) on evidence-based programs in child health and development with diverse populations (Bruner and Johnson, 2020; Cannon et al., 2017; Doyle et al., 2019; Einhorn Family Charitable Trust et al., 2016; Li and Ramirez, 2023; Institute of Medicine and National Research Council, 2014; NASEM, 2016; NASEM, 2019). From 2016 through 2023, InCK Marks, a national organization dedicated to advancing child health care transformation at the federal, state, and community levels, was funded by the Robert Wood Johnson Foundation (RWJF) to conduct extensive research in this area; the eight reports were all identified by the RWJF-funded InCK Marks initiative as those that delved most deeply into identifying exemplary evidence-based programs.
The RFI and synthesis of the noted reports identified over 60 different programs and practices operating within primary care, several with evidence of diffusion and scaling. Additional criteria for selecting exemplars of successful scaling, described in Section 2, are based on one of the eight noted reports that defined successful scaling as being scaled to more than 1,000 patients within pediatric primary care annually (Einhorn Family Charitable Trust et al., 2016). In addition, while the authors initially aimed to limit inclusion of literature to those published in the last 10 years, this produced a very limited number of both peer- reviewed publications and online gray literature; thus, this search parameter was revised to also include literature prior to 2014. The four selected core topics (parent engagement, implementation, sustainability and scalability, and policy and funding) went through an iterative vetting process to ensure that what is most meaningful to the identified key stakeholders would be reflected in the end product. Third, the contributing authors are from different sectors, including, but not limited to, academia, hospital systems, FQHC/safety-net health care systems, applied research entities, government, community-based organizations, and represent various disciplines (e.g., pediatrics and primary care, public health, education, health economics, prevention science, psychology, and public policy). Last, the authors’ direct engagement with parents, families, and children from marginalized populations has informed their individual and collective nuanced understanding and shared sense of urgency as to why this work is sorely needed now.
The equitable implementation framework (Figure 1, developed by Loper and colleagues (2021), serves as the guiding framework for review and synthesis of HPPC interventions, policies, and practices to This framework draws from the field of implementation science, which aims to bridge the gap between research evidence and real-world settings by examining the contextual factors that lead to successful uptake, scaling, and sustainability of programs, practices, and policies. Loper and colleagues (2021) call attention to how inequities, such as navigating power dynamics, excluding community members from co-creating interventions intended for them, as well as structural racism and other forms of oppression, are all part of the context in which interventions are delivered, but have not traditionally been addressed in implementation science. They define equitable implementation as “an explicit and intentional integration of implementation science and equity that attends to what is being delivered, for whom, and under what conditions; and how delivery should be tailored to best meet the needs of the focus population. Equitable implementation occurs when strong equity components—including explicit attention to the culture, history, values, assets, and needs of the community—are integrated into the principles, strategies, frameworks and tools of implementation science” (Loper et al., 2021). The authors apply this framework throughout this discussion paper as part of a concerted effort to focus on HPPC interventions in the context of marginalized youth, parents and families, communities, and the health care systems and settings that serve them.

FIGURE 1 | Elements of Equitable Implementation SOURCE: Metz, A., B. Woo, and A. Loper. Equitable implementation at work. Stanford Social Innovation Review 19(3):A29-A31. https://doi.org/10.48558/R793-6704.
This paper represents an initial in-depth synthesis of evidence-based, evidence-informed, and promising HPPC programs and practice changes that include one or more of the six elements of equitable implementation. The full list of change initiatives includes brief descriptions of the specific practice or program features and objectives, and is available to read online (InCK Marks, 2024). The identified interventions cover a wide range of populations, implementation settings, and foci within the primary practice, from direct training of the pediatric primary care workforce to integrated or co-located programs and referrals. In addition, the programs and practices vary in their degrees of efficacy and successful replication, diffusion, and adaptation within other practices or for other populations. These programs can be implemented within, or in coordination with, primary pediatric practice. When deployed alone or in conjunction with other interventions, they have the potential to strengthen parents’ ability to positively impact children’s cognitive, social, physical, and emotional development and well-being.
The programs share common elements: engaging and supporting parents, working with parents as respected partners and within parents’ cultural systems and communities, and providing parents specific skills to promote child development and emotion regulation (Wakschlag et al., 2024). The programs include or can be paired with mechanisms to systematically identify parenting strengths, vulnerabilities, and family stresses that the practice can also address. Last, while the list was vetted and approved by all contributors of this paper, the full preferred reporting items for systematic reviews and meta-analyses guidelines were not followed and is a potential limitation of the current discussion. It is possible that additional innovative practices exist but are not captured in this review. Nonetheless, the purpose of this paper is neither to be exhaustive nor definitive, rather to provide exemplars that show the range of HPPC innovations that currently exist and inspire further action.
Section 1: Incorporating Parent Voices in HPPC Intervention Design, Implementation, and Evaluation
Pediatric primary care is increasingly focused on advancing health equity and integrating lived experiences into the design and implementation of parenting programs. Foundational studies offer critical frameworks and methodologies for effectively involving parents and community partners in health research, a practice that enhances health equity and intervention effectiveness (Israel et al., 2012; Minkler and Wallerstein, 2011). This body of literature emphasizes the importance of engaging parents as participants and active partners in designing, implementing, and evaluating pediatric primary programs. Such involvement works to improve interventions to be culturally relevant, ethically sound, and more likely to be successfully adopted in community settings (Green and Kreuter, 2005; Lasker and Weiss, 2003). This participatory approach is reflected in recent literature on developing tailored and responsive parenting programs within pediatric primary care, aligning with the strategies to incorporate parent voices to tailor interventions to specific needs, such as emerging programs presented to the HPPC (NASEM, 2023; Emery Tavernier et al., 2024; Javier, 2023; Oo et al., 2024; Powell, 2023). This literature underscores the need to incorporate parent voices to ensure interventions are tailored to their needs. Recent literature highlights the pivotal role of health care researchers in connecting with community partners, demonstrating the multifaceted benefits of such engagements (Carman et al., 2013; NASEM, 2023; Powell, 2023). Carman and colleagues (2013) underscore the importance of engaging the parent voice at the point of care and in organizational design and policy decisions. This complements the push for health equity and tailored interventions in pediatric primary care. However, despite the critical importance of including multiple parent perspectives, the involvement of parents in research on HPPC interventions varies widely and is often inconsistently reported and disseminated (Gonzalez et al., 2018). For example, when parent involvement is highlighted, it is frequently measured by engagement metrics, such as attendance, program completion, or program satisfaction, rather than evaluating parents’ attitudes toward the intervention or its alignment with their prioritized needs and concerns (Bjørknes and Ortiz-Barreda, 2021). This is echoed in recent literature where Moon and colleagues (2024) suggest that engagement is multidimensional and highlights additional domains, such as trust and a working alliance, and Mehus and colleagues (2019) document parents’ desire for more engagement in those same domains. For the purposes of this discussion, parent engagement refers to the multidimensional domains including behavioral, attitudinal, and relational engagement of parents throughout the research continuum (Bjørknes and Ortiz-Barreda, 2021; Mehus et al., 2019; Moon et al., 2024).
This section presents innovative research that incorporates parent voice in program development, from conceptualization to implementation and evaluation. This section also highlights organizations and programs that are exemplars of incorporating parent voice into parenting interventions in primary care settings. Figure 2 is a visual that guides the review and discussion of partner (e.g., parent) involvement wherein programs can be placed vertically (according to the stage or stages of partner involvement along the research continuum) and horizontally (according to the level at which the partner’s voice is incorporated throughout each stage).

FIGURE 2 | Stages and Level of Partner Voice and Involvement in the Research Process SOURCE: Pollock, A., P. Campbell, C. Struthers, A. Synnot, J. Nunn, S. Hill, and R. Morley. 2019. Development of the ACTIVE framework to describe stakeholder involvement in systematic reviews. Journal of Health Services Research & Policy 24(4):245-255. https://doi.org/10.1177/1355819619841647. NOTES: The horizontal axis is material adapted from Pollock and colleagues (2019), who created the ACTIVE framework to describe the stakeholder and partner involvement level in the systematic review process. The vertical axis is not designed to represent the research process fully and may have additional or omitted stages, or may not follow these stages linearly depending on the type of intervention or practice being developed and the setting in which development or adaptation occurs.
What Supports Do Parents Want in Pediatric Primary Care?
Primary care health providers are an essential resource for support for parenting and management of common early childhood behavioral challenges, with parents consistently reporting high interest in receiving behavioral health resources through pediatric primary care (Mehus et al., 2019; Riley et al., 2021; Zimmermann et al., 2021). Research indicates that parents endorse several behavioral topics as being essential to address in pediatric primary care in the domains of emotion and conduct (e.g., anxiety, disruptive behavior) and healthy habits (e.g., eating, sleeping) (O’Dell et al., 2021; Riley et al., 2019). Themes from several primary care–based studies indicate that parents are interested in a variety of strategies for receiving behavioral guidance for parenting young children in the primary care setting, including meeting with integrated behavioral specialists and digital methods for accessing evidence-based materials (Mehus et al., 2019; Riley et al., 2019). In several studies, for example, parents preferred individual rather than group treatment (Fehr et al., 2020; Riley et al., 2019). The authors also acknowledge that the supports parents’ desire in pediatric care settings, including those reviewed here, are unlikely to be implemented without the foundation of increased provider training and organizational readiness to implement new practices effectively (Lau et al., 2015).
Parents indicate value in the pediatric care setting of learning about and being provided referrals to other resources and support related to parenting, such as child care and concrete, economic support (Spain et al., 2021). There is a small but growing body of research aiming to understand more about the types of supports and services and the content areas that parents are seeking in the pediatric primary care setting. A mixed methods work by Riley and colleagues (2019) suggests that although parents report a desire to receive more parenting support in primary care, they are most interested in services tailored to their family’s specific needs and values rather than universal guidance. This work also highlights the potential role of stigma in affecting preferences for parenting support. For example, parents reporting greater use of physically controlling parenting practices (e.g., corporal punishment) indicated increased stigma associated with receiving parenting support and preferred that visits addressing parenting and child behavior be integrated into existing medical appointments rather than scheduled as a separate visit. These themes highlight the need to offer multiple options for supporting parents in the pediatric primary care setting and universally promote such services to reduce stigma (Williams, 2020). However, one noteworthy gap in the literature to date is parents’ priorities, needs, and preferences, specifically regarding topics related to parenting adolescents. One exception is a qualitative study conducted by Ford and colleagues (2016) in which a racially diverse sample of parents of adolescents reported a strong desire for support from their children’s health care team on topics relevant to adolescent development and mental health. Parents of Black adolescents were most likely to express high interest in most health topics (e.g., dating, sleeping, parent–teen communication).
Many pediatric health care settings are also integrating screening and conversations with parents about health-related social needs (HRSN), and more family-driven resources to guide HRSN approaches in primary care are being developed to support practices. For example, written by families, the Family Voices and American Academy of Pediatrics (AAP) “Bright Futures Family Pocket Guide” enhances AAP’s anticipatory guidance, including recommendations and periodicity related to HRSNs, such as housing, household stress, caregiver strengths, and availability of social support (Hagan et al., 2017; Vickers et al., 2021). Several initiatives for families with Medicaid health insurance are underway to provide options for states to innovate and test models of supporting HRSNs within health care settings (Lee et al., 2022). Many parenting programs implemented in pediatric primary care, such as SafeCare and the Developmental and Legal Collaboration for Everyone (DULCE) have demonstrated success in engaging parents to support, not only parents’ interest in understanding specific parenting behaviors that influence children’s development, but other household factors for which support is available but many parents may not know about or access (Guastaferro and Lutzker, 2019; Sege et al., 2015).
Incorporating Parent Needs and Perspectives Throughout the Design and Evaluation Process
Integrating a health equity framework into pediatric primary care involves meticulous planning and genuine collaboration at multiple stages of health care intervention development. Drawing from recent programs like the Focus on Youth (FOY) + ImPACT adaptation, the Prescription for Play (P4P) initiative, and the Family Network Collaborative (FNC) model, it becomes evident that parent and family involvement should extend beyond traditional engagement metrics (Powell, 2023; Oo, 2024; CCSP, 2024). These programs exemplify a shift toward a more inclusive and participatory approach, aligning with the outlined levels of involvement, from one-time to hands- on approaches, ensuring that interventions are developed and refined to truly reflect the needs and preferences of the communities they aim to serve. The FOY + ImPACT program, specifically adapted to address the unique challenges African American youth face in Baltimore, demonstrates the effectiveness of involving parents and community members continuously and intensively throughout the intervention stages. This engagement spans from choosing the priority issues (i.e., substance use and sexual risk behaviors) to testing and refining the intervention, thus fostering a sense of ownership and alignment with community values (Powell, 2023). Similarly, P4P incorporates a hands- on approach by equipping pediatric care providers with tools to foster play and actively involve families in goal-centered play, which promotes play as a fundamental aspect of child development (Oo, 2024).
Furthermore, the FNC model introduces an approach that emphasizes direct family engagement, thereby enhancing early childhood and relational health by utilizing the lived experiences of families (CSSP, 2024). In the context of pediatric research, family engagement, which shares commonality with the definition of parent engagement used in this section, is further defined as the comprehensive involvement of families in setting research priorities, designing study protocols, and disseminating priority actions to ensure research aligns with patient and family needs and values (Tamburro et al., 2023). This involvement ranges from passive participation to active and deliberative roles, significantly enhancing the research process and outcomes by integrating the unique perspectives of families (Tamburro et al., 2023). Traditional engagement methods typically utilize professional intermediaries; the FNC model differentiates beyond the traditional by empowering family members to directly contribute to developing research priorities, refining consent processes, and formulating research agendas (Tamburro et al., 2023). This model embodies a genuine community-led approach, ensuring that families are integrally involved in decisions that impact them, thereby enhancing the authenticity and relevance of pediatric critical care research (Tamburro et al., 2023). By engaging families throughout the development, low implementation, and refinement stages of health interventions, models like the FNC model foster a deeper, more empathetic understanding of families’ challenges and leverage their insights to develop more effective and inclusive primary care systems. Tamburro and colleagues (2023) outline a comprehensive community-led model for involving families in critical care research, which can also be applied to primary care settings. This model underscores the importance of integrating family insights across all stages of health care—from development and implementation to refinement—to enhance the relevance and effectiveness of critical and primary care interventions. This commitment to intentional parent engagement facilitates a deeper connection with community needs and a more accurate reflection of diverse family dynamics in health programming.
Finally, the Children’s Hospital at Dartmouth- Hitchcock’s Purple Pod approach to supporting mothers with substance use disorders caring for infants was developed based on feedback from mothers, resulting in a model of strengths- based and trauma-informed care and employing a multidisciplinary team to help mothers and family members navigate health care and other services. Again, goal setting is designed through parent preferences and is conversational and realistic, emphasizing both mothers’ and infants’ well- being (AAP, n.d.b). By focusing on strength-based support and comprehensive care coordination, the program aligns with best practices in pediatric health by fostering an environment that supports maternal recovery and promotes healthier infant outcomes (AAP, n.d.b).
BOX 1 | Keystones of Development
The Keystones of Development (KoD) curriculum is a dual-pronged parenting and health care professional (HCP) provider technology-based intervention that uses several innovative parent engagement strategies to improve parenting interventions and parents’ experiences of those interventions in the primary care setting. This program is run out of the Mount Sinai Parenting Center in New York. From the outset, the program was closely tethered to parent voice through Zero to Three’s Millennial Connections results. Millennial Connections is a national survey of parents conducted in 2015, which sought to identify parents’ challenges, needs, and their opinions about the parenting support they currently receive. The results of this survey directly informed the design of both the parent-facing resources (e.g., what information should be presented to meet parent-identified needs and challenges) and the HPC trainings (e.g., how should HCPs share this information in ways parents would like to receive it). The KoD curriculum is now delivered annually to pediatric and family practice doctors across over 85 percent of pediatric residency programs and 36 percent of family practice residency programs in the United States; the training focuses on HCP training in critical developmental concepts and continues to grow (Martin et al., 2020). The data are promising: HCP trainees who participated in the KoD training showed greater confidence in interactions with parents and reported behaviors and decreased perceived barriers to promoting positive parenting in well-child visits (Hammond et al., 2022). This is an example of how even one-time parent involvement—during the problem formulation and prioritization of parent needs in the design of an intervention—can impact the relevance of a parenting program (Figure 1).
In Box 1, the Keystones of Development curriculum (KoD; Hammond et al., 2022) is highlighted as an exemplar of incorporating parent needs and perspectives throughout the design and evaluation process, as detailed in Figure 2.
Building on the success of the KoD initiative, Mount Sinai Parenting Center is now in the process of developing additional tools to meet the needs of parents, including the Sparks, a parent video series, co-designed with parents across the United States, with representation and parent input from Spanish-speaking parents, parents of children with disabilities, urban and rural parents, and African American parents. The creators of Sparks at Mount Sinai not only include parent voice in the initial design of the intervention, but they are also asking parents about their experience receiving parenting information through video format (e.g., if they feel the information is relevant to them and if they feel more confident in positive parenting having received the videos). Evaluation data are not available as of this writing because the intervention was launched in 2023; however, this is an example of “top and tail” parent stakeholder involvement (Figure 2). These interventions represent strong examples of how parent voice and preference can be integrated into the design and evaluation process when building effective parenting supports for primary care contexts.
Coker and colleagues’ (2016) PARENT (Parent-focused Redesign for Encounters, Newborns- Toddlers) program is a well-child care model that incorporates a health educator “parent coach” into well-child visits (Coker et al., 2016; Coker et al., 2023; Mimila et al., 2017). PARENT has been found to improve parents’ perceptions of the quality of care they received, including helpfulness and family-centeredness, as well as the parents’ report of their receipt of anticipatory guidance in well-child visits (Coker et al., 2016; Coker et al., 2023). Coker and colleagues (2009) began by conducting focus groups with parents of young children recruited through FQHCs to learn about parents’ perspectives on improving pediatric primary care delivery. Over the next 15 years, the research team continued to use community- partnered processes to engage parents throughout the design, testing, and implementation phases of the intervention development.
Summary
The authors’ review of existing programs shows greater intentionality with parent engagement in HPPC programs and practices, particularly in the selection of priority areas for the design or adaptation of interventions, and to a lesser extent, in the evaluation of those programs. Butler and colleagues (2020) provides a comprehensive review on parents’ perceptions of and experiences with these programs. Nonetheless, evidence documenting parent voice and involvement throughout the research process and the degree to which programs ultimately meet parents’ expressed needs are not widely disseminated, and methods and measures for obtaining this information through research and evaluation is sparse. This presents the opportunity to generate new research strategies to document parent voice along the continuum of program development and parenting intervention design and evaluation. As shown by the number of groups who are prioritizing parent voice, but for which those actions are not published or readily available, the authors encourage groups and organizations doing this work to more broadly disseminate strategies and actions through formal and informal channels to catalyze those efforts toward the goal of making parent voice a key component in shaping equity- driven parenting interventions.
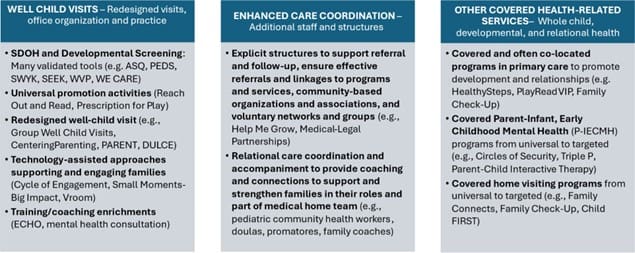
FIGURE 3 | Examples of Evidence-Based Programs and Practices Grouped by Child Health Transformation Elements SOURCE: Johnson, K., and C. Bruner. 2018. A sourcebook on Medicaid’s role in early childhood: advancing high performing medical homes and improving lifelong health. Des Moines, IA: Child and Family Policy Center. Available at: https://www.inckmarks.org/docs/pdfs_for_Medicaid_and_EPSDT_page/ SourcebookMEDICAIDYOUNGCHILDRENALL.pdf (accessed November 15, 2024). NOTES: Many more evidence-based models and programs exist that can contribute to and are consistent with health care transformation for young children.
Section 2: Research on Effective Implementation and Adaptation of HPPC Interventions
The principles of a medical home (i.e., family centered, compassionate, culturally effective, accessible, continuous, and comprehensive) and subsequent formulations for transforming pediatric primary care provide a strong conceptual framework for how primary care should relate to children, parents, and communities. However, some frameworks tend to stop short of describing specific programmatic and operational elements for successful transformation (or reflecting that different practices have different capacities in response). This section presents innovations in primary care to strengthen parenting that have demonstrated implementation feasibility within, or in coordination with, primary care practices serving children. Drawing from the description of “high-performing medical homes” for children, the innovations described here are organized by how they are structurally integrated into, or transform the process of, primary child health care (Johnson and Bruner, 2018):
- The structure of well-child visits and office practice configuration.
- The incorporation of staffing for enhanced care coordination as part of the medical home team, directed to parenting and the home environment.
- The provision of additional services covered under primary care to strengthen families and the safety, stability, and nurturing in the home environment.
Figure 3 shows these three core components of primary child health care, along with representative tools, programs, and practices. Within each component, the authors grouped innovations by the type of strategy employed. Programs and practices may vary in focus (e.g., universal, targeted toward specific concerns, or developmental stages) and the types of settings (e.g., hospitals and other large pediatric practices, community health centers, and smaller practices in rural settings) for which they would be a good fit. Many programs identified by this review could fit under multiple categories. For example, Family Check-Up 4 Health (FCU4Health) is both a parenting intervention and a care coordination model for connecting families to community services for economic and social needs (Smith et al., 2018). Examples of health systems that have incorporated or adapted programs and systems change efforts across all three components can be found on the InCK Marks website (InCK Marks, 2024). Collectively, these components demonstrate an extensive array of programs and services aligned with the principles of a medical home and its emphasis upon families as key contributors to healthy child development. Overall, they can advance primary child health care in fulfilling its fundamental mission to achieve healthy social, emotional, cognitive, and physical development in children by supporting effective parenting.
Programs and Practices under Well-Child Visits
The authors have grouped programs and practices that enhance visits, or “patient encounters,” into several different areas described below.
Validated pre-visit screenings gather information from families and have value when there is follow- up and response to potential concerns identified in the screening process. Some screening tools (e.g., Ages & Stages Questionnaires, Ages & Stages Questionnaires—Social-Emotional, and Parents’ Evaluation of Developmental Status) address the status of children’s overall healthy development across physical, social, and emotional development as a foundation for further anticipatory guidance during the visit and potential referral to services to address them (Squires et al., 1995; Squires et al., 2002). Other assessments (e.g., Safe Environment for Every Kid, Survey of Well-being of Young Children, and the Pediatric ACEs and Related Life Event Screener) check for social and economic factors or adverse child experiences and may lead to enhanced care coordination or further anticipatory guidance, follow-up by the practice, or parenting services in response to identified needs or concerns (Bucci et al., 2015). More specifically, the Well Visit Planner (WVP) incorporates questions about both the child’s development and social determinants and provides information to practitioners and to parents completing the planner, including helping parents prepare for the well-child visit by suggesting particular issues they should raise with their child’s practitioner as a result of the screening.
Several programs are aligned with practices that have reorganized the overall well-child visit to better support parents and families. Centering Parenting incorporates a provider- or staff-led parenting group into well visits following time spent in individual assessments (Dimovitz, 2023). DULCE includes an additional staff person in the well-child visit who can follow-up in engaging families and responding to health-related but not medical concerns (CSSP, 2019). These approaches might be most appropriate for larger practices given resources and larger clinic flows required to sustain them.
Reach Out and Read (ROR) and P4P represent two universal promotion activities that can be incorporated into well-child visits across a broad and diverse array of practice settings to help parents engage in nurturing, cognitively stimulating, and relationship-based activities with young children. ROR has a very large research base showing positive impacts on parenting and child development and has been widely and successfully implemented. Both ROR and P4P have shown the ability to be incorporated into the time generally allotted for well-child visits.
Some HPPC interventions employ specific technology enhancements. For example, the Cycle of Engagement, which is part of the WVP, incorporates the findings from the WVP into medical records, provides reminders of upcoming visits, and enables inter-visit feedback and updates regarding the child’s development. Vroom incorporates online tools to provide tips on parenting (Vroom, n.d.), while Small Moments Big Impacts provides videos on a wide range of topics around child development and parenting, for viewing in the visit itself with the practitioner and for accessing through a website (Small Moments Big Impacts, 2024).
Finally, programs that offer coaching and teaching for primary care staff offer additional consulting and support to practices. Mental health consultants, for example, can be bridges between practices and community providers serving their children and families to better respond to early mental health concerns. The Project ECHO (Extension for Community Healthcare Outcomes) model offers specialist and peer-learning opportunities for practitioners and families that offer the ability for continuous education and development (Weitzman Institute, 2024).
Programs and Practices under Enhanced Care Coordination
One of the principles of effective medical homes is to provide care coordination to all children and families that extends beyond the medical aspects of well-child and other office visits (Council on Children with Disabilities et al., 2014). This also is a requirement of Medicaid under its Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit. Some children and families require little or no such care coordination, while others require extensive coordination (e.g., due to their children’s complex medical conditions or the family’s complex social and relational health care needs) (Bethell et al., 2022; Bruner et al., 2018; Bruner, 2021b). In these instances, supporting child and family well-being necessitates much more than merely suggesting that parents contact other programs or services for help. It requires follow-up and sometimes advocacy or expert support to ensure essential services and supports are secured.
Medical–legal partnerships, suited to larger practices serving children and families whose economic status or special health needs require additional advocacy, have a long history of effectiveness in connecting families to community services and ensuring they are successful in applying for supports for which they are eligible, including housing, Social Security Insurance, Supplemental Nutrition Assistance Program,
Temporary Assistance to Needy Families, and other benefits (Martinez et al., 2017). The word “legal” is important, as it often requires substantial expertise to access some important services with specific eligibility requirements or to address legal aspects of resolving family situations that cause stress or hold families back. Particularly for smaller practices and family practitioners serving rural communities, Help Me Grow’s model’s of providing telephone care coordination for multiple practices offers an enriched and personalized linkage for both referrals and follow-ups to ensure participation and help for families to identify supports that best meet their needs (Miller et al., 2023).
While the medical–legal partnership and Help Me Grow’s enhanced care coordination tends to involve relatively brief encounters that provide specific responses to family needs, a growing array of care coordination efforts establish ongoing relationships of trust with children and families that are core to ensuring they are central to the medical home response. Allied health care professionals, such as pediatric promotoras, community health workers, family coaches, and doulas ideally take on multiple on-the-ground roles that strengthen family agency in nurturing their children, provide continuity and appropriate intensity of relational care with the child or family, serve as the bridge and liaison to culturally and linguistically responsive community resources and connections, and improve the capacity and cultural responsiveness of the primary care practice. While much of the research on this segment of the health care workforce has been directed to those working with adults, their long-term impact on both individual and population health is greatest for children (Barbosa and Alvarez, 2021; Bruner and Sullivan, 2022; CDC, 2024; Community-Based Workforce Alliance, 2021; Garfield and Kangovi, 2019; Lloyd et al., 2020; Zulu and Perry, 2021).
Programs and Practices under Other Covered Health Services
In addition to screening for, diagnosing, and treating medical conditions, pediatric care is responsible for screening for health-related concerns that include social determinants of health. Under the Medicaid EPSDT benefit, this requires implementing a broader range of reimbursable services. The highest level of support for parenting includes programs that focus on the development of parenting strategies to improve child physical and social-emotional health. These types of programs generally focus on positive parent– child relationships, communication, and effective discipline practices, and may include additional components based on family circumstances (e.g., divorce or bereavement). These programs vary based on the level of need and can be implemented within or outside of the clinical setting (Buchanan et al., 2023; Leslie et al., 2016). For example, some are applicable to all families (e.g., Guiding Good Choices; Scheuer et al., 2022), whereas others are more selective and indicated responses that can be tailored to the level of need for individual families (e.g., FCU4Health; Berkel et al., 2021).
To varying degrees, states have expanded their child health coverage under Medicaid to include evidence-based programs that support effective parenting as a pivotal pathway in children’s healthy development. This includes coverage for HealthySteps, PlayReadVIP, and other specific programs directed to equipping parents, through their nurturing and supervision of children, to meet the child’s health and development needs. Primary care settings with integrated behavioral health have been successful in billing for some components of parenting programs (e.g., assessments and parenting modules) using current procedural terminology codes; however, other components (e.g., preparation time) are not billable. Parenting programs that focus on whole child health, like FCU4Health, may have financial incentives for primary care organizations through EPSDT and improving Healthcare Effectiveness Data and Information Set scores (Berkel et al., 2020).
There has also been growing use of Medicaid to cover home visit programs and services, particularly those that have been designated as evidence-based within the Health Resources and Services Administration’s Maternal, Infant, and Early Childhood Home Visiting (MIECHV) program (Health Resources & Services Administration, 2024). These extend from near universal and check- in home visits (e.g., Healthy Foundations) to more intensive home visits targeted to families with the greater vulnerability (e.g., Nurse Family Partnership, Healthy Families, and Parents as Teachers) and evidence of wide diffusion (Eckendrode et al., 2017; Guastaferro et al., 2018; LeCroy et al., 2020). Coverage may also include services (frequently in the form of patient support groups) directed to providing additional care and information around specific health conditions in the child (e.g., autism, spinal bifida, or other diseases) that require special and ongoing caregiver attention. Other programs and services that support parents in their role of strengthening their child’s social and emotional development include those applicable to all families, such as the Positive Parenting Program (PPP), and those that are more selective and indicated responses to identified concerns (e.g., Circle of Security, dyadic parent-child therapy). A summary of all programs and services mentioned in this section, including their respective goals and core components, can be found on the InCK Marks website (InCK Marks, 2024).
Factors to Consider in Program Selection and Implementation
For any given practice or setting, the approach needs to be tailored to the particular population served, resources available within the practice and in the broader community, and the capabilities and configuration of the practice staff (Berkel et al., 2021; Buchanan et al., 2023; Matson et al., 2022). Understanding the attributes or qualities that make them effective can help practices do this (Bruner, 2006; Dunst, 2021; Kinney, 1994; Schorr and Schorr, 1989; Schorr et al., 1991). Referring and helping engage parents with agencies and organizations outside the practice walls may be particularly important for smaller practices that may not have the patient base to warrant expanding their own staffing to provide additional services.
For settings serving families whose trust in the system is low, it will be vital to have someone associated with the practice whom they do trust, and who can engage them in the practice and in accessing other programs and services (Mehus et al., 2024). Practices will want to take special care to employ programs and approaches that pose barriers to family participation (e.g., childcare, transportation, time burden) and thereby potentially increase disparities in care and children’s health outcomes (Berkel et al., unpublished; Wright et al., 2022). Additionally, there will be start-up costs and ongoing investments in providing these additional supports to parents, as well as expanding outreach efforts to parents to be aware and make use of these programs and services (Jordan et al., 2019). The biggest investment of time and staffing will be in the enhanced care coordination that effectively responds to social, behavioral, educational, and relational determinants of health and meaningfully connects families to health-related services.
As programs spread beyond innovators and early adopters, practices will often require coaching and support from trained colleagues and experts in the programs (Greenberg, 2006; Rogers, 2010). They often will have to manage new workflows, new involvement of parents and community partners, financial modeling, and additional training of staff in supporting healthy parenting in the overall practice. In both instances, there is some potential to braid and blend existing financing mechanisms and resources, such as federal block grants that provide substantial state flexibility in use (e.g., Medicaid 1115 demonstration waivers). However, increased funding for these services as part of primary child health care, particularly through Medicaid and its EPSDT benefit, would greatly enhance sustainability (Ascend at the Aspen Institute et al., 2019; Bruner and Johnson, 2018; Bruner et al., 2021). Overall, providing greater supports for children and families through primary care requires a shift away from cost containment toward an investment in or value-based approach to care that increases direct payments to practices (Bruner and Hayes, 2023; Bruner et al., 2017; Counts et al., 2018).
Summary
The programs and practices described in this section show the innovation and progress that has been achieved in operationalizing the principles of a medical home, implementing the field’s guidelines for well-child care, and responding to the whole child and the child’s relational health needs. While far from exhaustive in identifying all evidence- based practice and program innovations, it shows the readiness of the field to take bold steps to both broaden and deepen primary pediatric practice to advance healthy child development.
Section 3: Pathways to Ensure Sustainability and Scalability of HPPC Interventions
The wide range of evidence-based programs and practices implemented as part of, or in association with, the medical home presented in Section 2 of this discussion paper is a strong foundation for expansion to universal promotion of parent–child interactions that support early relational health and healthy child development. There is a large literature base on scaling within health care generally with the most widely used definition of scaling being “deliberate efforts to increase the impact of successfully tested health innovations so as to benefit more people and to foster policy and programme development on a lasting basis” (Coroa et al., 2023). This was introduced in 2010 alongside a scaling framework that made the distinction between horizontal scaling in the form of expansion or replication of a program and vertical scaling that comprises institutionalization through policy, political, legal, budgetary, or other health systems change (World Health Organization and ExpandNet, 2010). It also lists four elements to be considered as part of a scaling strategy: dissemination and advocacy, organizational process, cost and resource mobilization, and monitoring and evaluation.
Scaling an evidence-based or evidence-informed program or practice via the established pediatric primary care system that provides a ready-made platform for universal reach within the United States seemingly obviates many of the challenges of expansion. In reality, the variability in state and health system policy and practice, the multitude of pediatric clinic types and contexts, and the diversity of patients served introduces a complexity that is challenging to navigate. A previous review of programs that have strong evidence for efficacy when delivered through pediatric primary care in a local or pilot context identified challenges with wide-scale implementation that are aligned closely with the four elements required for successful scaling listed above with one additional element: adapting and translating to appropriate contexts, cultures, and demographics (Einhorn Family Charitable Trust et al., 2016).
Strategies for Successful Scaling
Successful scaling of a program or practice within pediatric primary health care only occurs as a result of strategic and intentional institutionalization of a program or practice through policy, budgetary, or other health systems change. While no comprehensive scaling strategies have been defined, several publications provide evidence for strategies that address the various challenges of universal expansion within pediatric primary health care and are detailed below.
Awareness and dissemination, as well as securing critical buy-in from clinicians, are most successfully achieved through inclusion or alignment of a practice or elements of a program in the Bright Futures Guidelines, the single unifying component used throughout pediatric health care. Bright Futures is a national health promotion and prevention initiative, led by the AAP and supported by the Maternal and Child Health Bureau at the Health Resources & Services Administration. It provides theory-based and evidence-driven guidance for what should be covered in each of the well-child visits for children from infancy to adulthood (Committee on Practice and Ambulatory Medicine, 2023). Similarly, the production of an AAP policy statement seems to be another successful dissemination strategy (Council on Early Childhood et al., 2014). The combination of these two strategies is a key ingredient in influencing what is considered of value in pediatric primary care and in helping toward recognition for billing.
Successful scaling requires maintenance of fidelity of practice or program delivery, including provision of online or in-person training, use of professional accreditation to encourage training uptake by clinicians, and provision of supplementary training or quality improvement projects to reinforce high quality practice. This has been most successfully achieved by programs that coordinate training through a national center and with ongoing local technical support offered through an affiliated infrastructure like ROR, as discussed in Box 2 (Garbe et al., 2023). Training residents is another successful tactic of improving practice as done by Mount Sinai Parenting Center and discussed in Box 3 (Hammond et al., 2022). Allowing for inevitable variation in the delivery of a program and identifying the active ingredient for impact as a focus for future training is critical in the scaling process (Jimenez et al., 2023; Piccolo et al., 2023). Although not documented, maintaining fidelity of practice or program delivery at scale requires an efficient means of capturing program data at scale.
BOX 2 | Reach Out and Read
After many years of organic growth, for the last 10 years, ROR has intentionally expanded and strengthened an affiliate infrastructure as a means of supporting growth with fidelity of delivery of the model that promotes positive, language-rich parent/caregiver–child interactions through shared reading. The effectiveness of this strategy in a real-world setting of diverse pediatric environments and a racially and ethnically diverse patient population was demonstrated in a publication in 2023, which considered more than 100,000 parent surveys completed at 427 clinics in North and South Carolina from 2014 to 2019 (Garbe et al., 2023). Analysis showed that families exposed to ROR were 27 percent more likely to read to their children every day and even more likely to use strategies to engage with their children when reading aloud together. ROR is currently delivered by 36,000 clinicians at 6,200 clinics throughout the United States.
BOX 3 | Mount Sinai Parenting Center
The Mount Sinai Parenting Center addressed a call from pediatric clinicians for support in training residents about parenting skills (Martin et al., 2020) by developing the Keystones of Development curriculum, a free, self-directed, 4-hour online course to all providers, along with faculty resources to support buy-in and integration into training. This curriculum has been successfully scaled to over 460 residency training programs across the United States and enrolls over 4,000 residents each academic year (Hammond et al., 2022).
Ensuring appropriateness and fit based on diverse contexts, cultures, and demographics is another critical consideration when scaling a practice or program. There is evidence of continued impact of several programs as they were scaled across a variety of clinic types with diverse patient communities in different contexts (Carson et al., 2019; High and Klass, 2014; Hughes et al., 2016, Javier et al., 2023; Perrin et al., 2014; Roby et al., 2021).
Financial barriers exist in both the process of scaling the intervention and ensuring sustainability at scale. Philanthropic grants are often the source of funding for piloting and initial growth of an organization, but it is necessary to develop public funding mechanisms to secure sustainable, universal program or practice implementation. Strategies adopted to develop public funding mechanisms include identifying billing and coding opportunities for the various services offered through the program (aligning services offered with Bright Futures recommendations that have attached billing codes), public and state-specific funding opportunities, and advice about making business plans (Crane et al., 2023; Sepulveda et al., 2021; Webster-Stratton and McCoy, 2015; Zero To Three, 2024). There is no published documentation of the wide-scale use of these funding mechanisms. A more detailed discussion about policy and financing levers for enhancing scalability and sustainability is included in Section 4 of this paper.
Collaborative Initiatives
As highlighted in Section 2 of this paper, there is growing interest in the impact of a combination of programs (often called “bundling”) that operate together either within the medical home or in connection with additional community programs with the intention of offering holistic parenting support for the diversity of families that make up the American population. Scaling of such collaborative approaches are generally instigated at the state or health systems level, which facilitates solutions to financial and advocacy/awareness challenges, but the operational and evaluation challenges are significant (see Box 4; McCord et al., 2024). Literature review reveals that, like evidence of scaling for individual programs, there is very little documentation of successful scaling in either the peer-reviewed or gray literature.
BOX 4 | 3-2-1 IMPACT (Integrated Model for Parents and Children Together)
3-2-1 IMPACT (Integrated Model for Parents and Children Together) is an initiative to transform the delivery of pediatric primary care within New York City health hospitals by combining the impact of evidence-based and evidence-informed interventions and supports (e.g., HealthySteps, ROR, Video Interaction Project, community health workers, social workers, and psychiatrists) to substantially improve child and maternal health outcomes and positively impact health disparities. The strategies used to launch and sustain the model included coalition building and sustained advocacy at the state, city, and health system levels, and collaborative implementation and clinical workflows with an electronic medical record build that managed the complexity. Long-term sustainability is being addressed through early childhood-focused advanced payment models and working with contracted Medicaid managed care plans. Over three years, the IMPACT initiative was fully implemented in three practices with many core components scaled systemwide, reaching over 11,000 children aged 0 to 3. Preliminary data for IMPACT sites demonstrate earlier ages at completed referral over the first year and mitigation of poverty and race and ethnicity-related disparities in the referral process, with increased referrals over the first year for the lowest income patient cohort (50 percent vs 40 percent) and for Black and Latino children (11 percent increase vs 3 percent citywide) according to McCord and colleagues (2024).
Research that Provides Evidence of Scalability
Given the strong foundation of promising programs and practices aimed at strengthening parenting delivered within or associated with the pediatric medical home, it is disappointing that there is so little evidence of impact at scale. This leads to scrutiny of the research practices that are employed to demonstrate scalability. The majority of research and evaluation on the impact of programs for young children and families has been conducted in the context of highly controlled studies (Fisher et al., 2020). Unfortunately, the few efforts of evaluation of scaled programs have produced mixed results, raising questions about the impact of programs as they scale (Besharov, 2024). In addition, there has been growing demand to increase the speed by which research moves into practice, but with little progress in accelerating the scale of research innovations (Shelton et al., 2018).
Use of scientific methodology that answers causality questions rather than measuring impact in real-world situations hinders scaling. Specifically, the focus on internal validity (or the degree to which causal evidence can be demonstrated with certainty) over external validity (or the generalizability of the results to different contexts and populations) has resulted in the inability of a large swatch of evidence-based programs to successfully evaluate scalability (Deaton and Cartwright, 2020). In the traditional research-to- practice paradigm, programs scale through strong adherence (i.e., fidelity) to program implementation as conducted by the original research. Although in theory this adherence allows for generalizability to the context in which the program is implemented, in practice it serves as a barrier to scaling. There are also equity concerns with traditional research methodology in that programs and innovations are often designed in the context of well-resourced hospitals and clinics and validated with convenience samples (Bruno and Iruka, 2022).
To address challenges of program fit and issues of scaling, there has been an increasing focus on adapting programs for different populations. For instance, Administration for Children and Families Tribal Home Visiting Program is the cultural adaptation of evidence-based home visiting practices for tribal families (Hiratsuka et al., 2018). This program has developed strong methods on how evidence-based programs can be more effectively scaled through systematic adaptation processes. In addition, the recently created Engagement in Action (EnAct!) framework (Figure 4) provides a comprehensive national model on how to scale strategies, innovations, and policies to promote child flourishing (Bethell et al., 2023). The EnAct! framework has spurred the creation of the Health Resources & Services Administration’s Early Childhood Developmental Health Systems Evidence to Impact Center (ECDHS, n.d.), which serves to build strong early childhood systems through scaling and adapting evidence-based strategies.
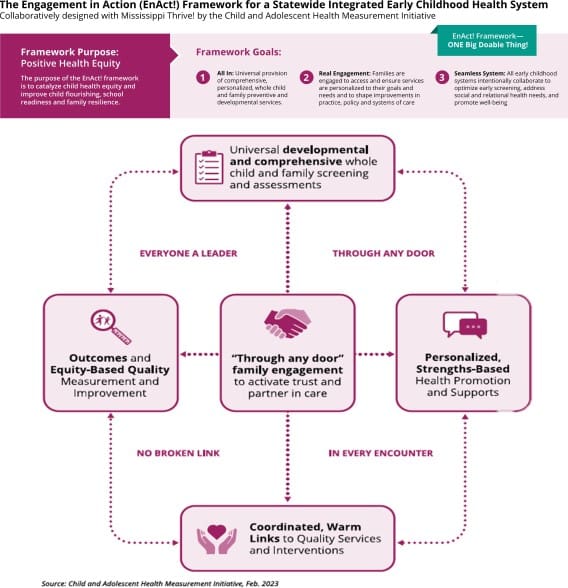
FIGURE 4 | Engagement In Action (EnAct!) Framework Purpose, Goals, Approach SOURCE: Bethell, C., S. Buttross, J. Schiff, D. Bergman, H. Hanna, S. Oppenheim, M. Bailey, R. Patterson, and N. Cattrell. 2023. The Engagement in Action (ENACT!) Framework. Available at: https://www.cahmi.org/our-work- in-action/engagement-in-action/EnAct!Framework (accessed November 11, 2024).
A growing method of quickly generating research insights that can be incorporated into practice is the establishment of Practice-Based Research Networks (PBRNs), a group of primary care clinicians and practices that work together to answer community-based health care questions and translate research findings into practice (Rhyne and Fagnan, 2018). PBRNs allow for a greater focus on external validity, as program innovations are tested in the contexts in which they would be scaled. The Agency for Healthcare Research and Quality has developed a PBRN initiative recognizing the importance of these networks to engage providers in developing and testing practices in the clinics in which they work. Two examples of PBRNS in pediatric primary care include the GROWBABY Research Network (Viglione and Boynton-Jarrett, 2023), which is based within the Center Parenting program, and the Early Relational Health Research Network, based within the ROR program (Dumitriu et al., 2023).
Measurement also plays a critical role in conducting research at scale. The focus on internal validity has also led to the development of hundreds of validated measurement tools to assess the quality of maternal and child health. However, these measurement tools are often primarily designed to be used in the context of rigorous research studies and are difficult and time consuming to administer in the field. As a program moves from supporting individual children and families to supporting relational health and resilient communities, the measurement tools utilized must change. To address these challenges, there are efforts to reconceptualize child and family well-being outcomes and the related measures toward child flourishing (Bethell et al., 2019). Also, over the last several years as focus has developed around population health, several population- level measures of early childhood development have been created. For example, The Healthy and Ready to Learn measure is a parent-reported indicator that tracks the development of children ages 3 to 5 and is currently included as part of the National Survey of Children’s Health (Ghandour et al., 2024). A very promising tool for younger ages is the Kidsights Measurement Tool, which measures a child’s development from birth to age 5 in four areas: motor, language, cognitive, and social/emotional development (Waldman et al., 2023). These emerging tools that are designed to be implemented at scale offer a compelling opportunity to evaluate and understand the impact of scaled programs.
Summary
Increased understanding of the importance of positive parent-child relationships in early childhood on a child’s development and long- term health and well-being demands a focus on bringing programs and practices that have been demonstrated to strengthen parenting practices through, or in association with pediatric primary care to population-level delivery. Online review of the programs outlined in Section 2 of this paper, along with informal connection with eight of them revealed that there is a significant level of such work in progress and many promising scaling strategies. However, the limited documentation of these initiatives in either peer-reviewed or gray literature poses a significant barrier to the dissemination of successful scaling strategies in this field. Acceleration of this work would be achieved by creating opportunities for informal exchange of learning about strategies at the same time as popularizing research methodology that more effectively provides evidence for the scalability of a program or practice.
Section 4 and Conclusion: The Role of Federal Policy and Funding in Supporting HPPC Innovation and Diffusion
The first section emphasized the particular role parents can and need to play as partners and participants in HPCC intervention design, planning, governance, research, and accountability. The second section summarized a broad and deep array of evidence-based programs and practices that have shown efficacy and promise for advancing HPPC, including training of the pediatric primary care workforce, capacity building for parents, as well as co-location of programs and referrals. The third section described key contributing factors to move from exemplary and often small-scale innovation and implementation to fidelity of replication and adaptation and broader spreading and scaling them. In looking ahead, the authors believe the health care community is at the point where public policies and funding (the fourth and concluding section of this paper) are needed to put what health care professionals know into much greater practice. The field now has many innovations worthy of further diffusion, a significant and growing number of innovations which have enlisted early adopters, and recognized leaders in the field which advocate for such practices to become the future standard of care (Rogers, 2010). The next stage in diffusion of innovation is to move to an early majority of practices, where there is a readiness to take action, but those actions require much greater and fully sustainable investments and commitments of financing. Those in the early majority will not take on the risk of innovators and early adopters but require full support and assurances and financing to do so.
Many of the critical design and implementation issues—related to adherence to overall principles and the fidelity of replication and adaptation of programs and ensuring parent voice (described in each previous section)—must ultimately occur at the state and community levels, but these also require federal support and direction and to ensure all states participate. In addition to ongoing costs to sustain program changes, there needs to be upfront expenditures and start-up costs to ensure fidelity and support continuous learning. These should draw from the field of implementation science.
This section specifically focuses on the role of federal policy in increasing funding to advance HPPC. More than half of all public investments in providing child health primary care come from the federal government—through Medicaid and Children’s Health Insurance Program (CHIP) and through the financing of FQHCs. A much larger percentage of children most vulnerable to compromised health outcomes due to social determinants and parental stress and parenting limitations are covered through federal health coverage programs. Much of the funding, particularly in the earliest years of a child’s life, for other health-related services advancing child health (home visiting, Part C of the Individuals with Disabilities Education Act, Linking Actions for Unmet Needs in Children’s Health, Early Childhood Comprehensive Systems, and for other Maternal and Child Health Bureau programs, and the block grant) comes from federal funding (Bruner and Johnson, 2018). Put simply, at the federal level there are two primary ways for Congress and the administration to support increased investments in evidence-based programs and practices that promote HPPC. These are through: (1) direct funding for HPPC programs or practices, including more specific inclusion of those programs and practices within existing funding for primary care; and (2) requirements, incentives, or new options under Medicaid and CHIP to cover those programs and practices as a part of primary care.
Recommendations for Direct Funding
The following represent proposals that different organizations and leaders in the primary child health field have proposed:
- InCK Marks’ sign-on letter to the administration recommending establishing a new block grant or expanding the maternal and child health services block grant to strengthen community and public health responses that provide financing, with a specific focus on pediatric community health workers’ capacity building (InCK Marks, 2021).
- A joint statement from child health organizations on Policy Options for Improving Child Wellbeing by Promoting Evidenced- based Parenting Interventions in Primary Care (AAP et al., 2021).
- Specific efforts such as the Black Maternal Health Momnibus Act (Underwood and Booker, 2020) to reduce maternal mortality and morbidity that provide additional support for a number of actions in the perinatal period to improve maternal and child health.
- InCK Mark’s sign-on letter recommending expanded start-up and diffusion funding for primary child health care by the Center for Medicare and Medicaid Innovation (CMMI) and InCK Marks’ sponsored sign-on letter to the Administration for changes to the CMMI statute to explicitly direct greater funding to child health.
- A direct increase in funding for MIECHV, for Linking Actions for Unmet Needs in Children’s Health, or for children’s mental health that includes language for connecting that with primary child health care.
- Expansion of work to establish metrics for primary child health practice that relate to safety, stability and nurturing in the home and early childhood attachment and early childhood attachment and development.
- Additional direct funding for workforce training and technology to build the skills and understanding of those in the primary care health system.
Recommendations for Medicaid (and CHIP) Incentives
Under incentives or new options under Medicaid and CHIP, this includes providing an enhanced Medicaid reimbursement match, such as Federal Financial Participation (FFP), for programs and services (including office visits) that promote healthy parenting in primary care and broadened administrative claiming for the training and technical assistance and support to design and implement them. The following represent proposals that different organizations and leaders in the primary child health field have proposed:
- InCK Marks’ sign-on letter to the Administration recommending enhanced federal financial participation for states establishing enhanced reimbursement to practices which operate as high performing medical homes (InCK Marks, 2021).
- Recommendations from the American Public Health Association, the Penn Center on Community Health Workers, the Children’s Partnership, and the Community-Based Workforce Alliance to include community health workers within Medicaid financing (Barbosa and Alvarez, 2021; Bruner and Sullivan, 2022).
- Enhanced FFP for FQHCs who enrich their child health primary care to incorporate additional parent strengthening services and activities.
- Use of administrative claiming and expanded FFP to incorporate broader metrics framework and support additional screening and follow-up services and to support a wide range of training and continuous improvement activities.
Additional Suggestions for Direct Funding and Medicaid (CHIP) Incentives
Funding must support both universal approaches and ones targeted to specific populations, both for children with specific medical conditions and those with health-related social needs requiring attention. Further, federal funding to increase use and diffusion of such programs and practices should ensure that children and families’ voices and participation are part of the medical home and support effective referrals, follow-up, and collaboration with other services in the community to which children and families are entitled. The following are additional suggestions for how federal funds can be used to expand specific programs and services:
- Provide parent education and support advancing healthy child development (e.g., HealthySteps, DULCE, PlayReadVIP, patient support groups).
- Increase the attention to supporting parenting in primary care visits (e.g., ROR, 4P, WVP/Cycle of Engagement).
- Hire staff dedicated to coordinating referrals to other services including earlier responses (e.g., Medical–Legal Partnerships, Help Me Grow).
- Expand nonmedical relational health care to children and their families to strengthen the safety, stability, and nurturing in the home and attention to the whole child (e.g., community health workers, doulas, family navigators, youth engagement workers).
- Invest in training and technology to foster more integrative and effective responses through building skills and understanding of those engaged with children and families (e.g., ECmental health consultation).
Such funds also can provide funding for more systemic responses by supporting primary care practices to strengthen their practice and workforce capacity across the components of primary well- child care visits, enhanced care coordination, and providing additional healthy parenting services (see Figure 3).
This work does not need to start from scratch; as noted in the recommendations above, there already are champions in Congress and the administration and robust specific financing recommendations to dramatically accelerate actions in the field. There are leaders in the child health field—at the administration, practice, and policy levels—who have advocated for transformational investments on the basis of their value, role in improving population-level health, and contribution to rectifying racial and other health inequities.
Building Consensus, Messaging, and Mobilization
While different innovators and exemplary practices can and should work to further refine their efforts and diffuse them to others, federal financing should be flexible in enabling practices to select and adapt programs and practices that best fit their needs. The authors have compiled a comprehensive, though not exhaustive list of evidence-based practices that practices can consider (InCK Marks, 2024). Financing also needs to be of sufficient scale to really move toward that early majority of practices, including supporting practices in planning and development. The framework established in the 2021 InCK Marks sign-on letter offers five specific areas where such investments should be made (InCK Marks, 2021).
Limitations
Due to resource and time constraints, the authors opted to conduct an in-depth environmental scan, which the authors acknowledge as the main limitation of this discussion paper. As previously noted, the authors recognize that the methods used for the literature review are not a substitute for a more comprehensive review of the literature with inclusion/exclusion research criteria. A future, more extensive scoping or systematic review would further deepen understanding of HPPC programs and practices and assist in identifying programs and practices that are most impactful and for which settings, populations, and desired outcomes.
As the number of children in the United States continues to grow, with 1 out of 5 (74 million) of the country’s population being under the age of 18, and more than half of young people in 14 states and the District of Columbia being children of color (US Census Bureau, 2023), the critical role of federal investments in HPPC interventions and related research is inherently linked to advancing health equity. Moreover, as the authors noted in the beginning of this paper, the compelling evidence in the Surgeon General’s Advisory on the Mental Health & Well-Being of Parents highlights the mental health challenges of parents and its impact on child well-being, which has been further exacerbated by the negative social and economic aftermath of the COVID-19 pandemic, further adds to the need for policy to move with urgency in funding and strengthening primary care systems in their efforts to support healthy parenting, so that all youth, and their parents, can thrive.
Join the conversation!
![]()
New from #NAMPerspectives: The State of Healthy Parenting in Primary Care Interventions in Advancing Health Equity. Read now: https://doi.org/10.31478/202503a
![]()
A new #NAMPerspectives discussion paper from @theNAMedicine takes a critical look at existing efforts to advance the field of healthy parenting in primary care by reviewing established and promising interventions. https://doi.org/10.31478/202503a
Download the graphic below and share on social media!

References
- AAP (American Academy of Pediatrics). n.d.a. Medical home. Available at: https://www.aap.org/en/practice-management/medical-home (accessed May 30, 2024).
- AAP. n.d.b. Promising practices. Available at: https://www.aap.org/en/patient-care/opioids/maternal-infant-health-and-opioid-use-program/promising-practices/ (accessed April 30, 2024).
- AAP, Mental Health America, Trust for America’s Health, Zero to Three, National Prevention Science Coalition, Center for the Study of Social Policy, and Coalition for Behavioral Health. 2021. Policy Options for Improving Child Wellbeing by Promoting Evidenced-Based Parenting Interventions in Primary Care. Available at: https://parentsforum.org/wp-content/uploads/2021/04/HPPC-PolicyOptions-9-20.pdf (accessed November 11, 2024).
- Ascend at the Aspen Institute, BrunerChildEquity, Center for Health Care Strategies, Center for the Study of Social Policy, Georgetown University Center for Children and Families, Johnson Group Consulting, National Institute for Children’s Health Quality, and Zero to Three. 2019. Opportunities for Medicaid to Transform Pediatric Health Care for Young Children to Promote Health, Development, and Health Equity. Available at: https://nichq.org/sites/default/files/resource-file/Medicaid%20and%20Early%20Childhood%20Consensus%20Document_%20Final%20September%202019.pdf (accessed November 11, 2024).
- Barbosa, G., and M. E. Alvarez. 2021. Community Health Workers Advancing Child Health Racial Equity. Available at: https://childrenspartnership.org/wp-content/uploads/2021/07/TCP-Community-Health-Workers-Final-Single-Pages-1.pdf (accessed November 11, 2024).
- Berkel, C., E. Fu, A. J. Carroll, C. Wilson, A. Tovar-Huffman, A. Mauricio, J. Rudo-Stern, K. J. Grimm, T. J. Dishion, and J. D. Smith. 2021. Effects of the family check-up 4 health on parenting and child behavioral health: a randomized clinical trial in primary care. Prevention Science 22(4):464-474. https://doi.org/10.1007/s11121-021-01213-y.
- Berkel, C., J. Rudo‐Stern, M. Abraczinskas, C. Wilson, F. Lokey, E. V. Flanigan, A. Juan , T. J. Dishion, and J. D. Smith. 2020. Translating evidence-based parenting programs for primary care: stakeholder recommendations for sustainable implementation. Journal of Community Psychology 48(4):1178-1193. https://doi.org/10.1002/jcop.22317.
- Berkel, C., K. Samaddar, K. McWilliams, G. Sioseth, J. Molina, V. Hernandez, and L. A. Rodriguez. n.d. “RE-AIMing for health equity: using RE-AIM to evaluate equitable implementation of the family check-up 4 health program in primary care settings” (unpublished manuscript, June 5, 2024). Microsoft Word file.
- Besharov, D. J. 2024. Program evaluation’s path to greater policy relevance: learning from rossi’s iron Laws. Evaluation Review 48(3):403-409. https://doi.org/10.1177/0193841×241238031.
- Bethell, C., S. Buttross, J. Schiff, D. Bergman, H. Hanna, S. Oppenheim, M. Bailey, R. Patterson, and N. Cattrell. 2023. The Engagement in Action (ENACT!) Framework. Available at: https://www.cahmi.org/our-work-in-action/engagement-in-action/EnAct!Framework (accessed November 11, 2024).
- Bethell, C. D., A. S. Garner, N. Gombojav, C. Blackwell, L. Heller, and T. Mendelson. 2022. Social and relational health risks and common mental health problems among US children. Child and Adolescent Psychiatric Clinics of North America 31(1):45-70. https://doi.org/10.1016/j.chc.2021.08.001.
- Bethell, C. D., N. Gombojav, and R. C. Whitaker. 2019. Family resilience and connection promote flourishing among US children, even amid adversity. Health Affairs 38(5):729-737.
- Bjørknes, R., and G. Ortiz-Barreda. 2021. Are the voices of parents heard? A scoping review of satisfaction in parenting programs. Evaluation and Program Planning 88:101928. https://doi.org/10.1016/j.evalprogplan.2021.101928.
- Bruner, C. 2006. Developing an outcome-evaluation framework for use by family support programs. In Family support as reflective practice. London, UK: Jessica Kingsley Publishers. Pp. 237-249.
- Bruner, C. 2021. Scope and scale: developing a risk/opportunity strategy for young children and their families to achieve population health. Working Paper Series No. 9, InCK Marks Initiative. Available at: https://www.inckmarks.org/docs/newresources/Oct2021/WP9ScopeandScale.pdf.
- Bruner, C., N. Z. Counts, and P. Dworkin. 2017. Alternative payment models for pediatrics: operationalizing value-based care over the life course. Available at: https://www.inckmarks.org/docs/keyissues/ALTPAYMENTMODELSjointMHAHMGCFPC.pdf (accessed June 15, 2024).
- Bruner, C., and M. Hayes. 2023. Federal health policy requires child health investment focus. Health Affairs Forefront. https://doi.org/10.1377/forefront.20230920.430993.
- Bruner, C., and K. Johnson. 2018. Federal spending on prenatal to three: developing a public response to improving developmental trajectories and preventing inequities. Available at: https://cssp.org/wp-content/uploads/2018/08/CSSP-Prenatal-to-Three.pdf (accessed May 21, 2024).
- Bruner, C., and K. Johnson. 2020. Young child health transformation: what practice tells us. Child Health Care Transformation Series Working Paper, InCK Marks. Available at: https://www.inckmarks.org/webinars/InCKMarksPracticeTransformationComponentfinalpdf.
- Bruner, C., K. Johnson, C. D. Bethell, P. Dworkin, M. Kotelchuck, E. C. Perrin, J. S. Shaw, M. N. Trefz, and R. Whitaker. 2018. Next steps in family-focused screening to address social determinants of health for young children in primary care. Available at: https://cahmi.org/docs/default-source/resources/next-steps-in-family-focused-screening-to-address-social-determinants-of-health-for-young-children-in-pediatric-primary-care.pdf?sfvrsn=a3bfba5b_0 (accessed June 15, 2024).
- Bruner, C., and E. Sullivan. 2022. Why kids and why community health workers? Advancing primary child health care practice transformation and community health responses to rectify racial inequities and improve population health. Working Paper, InCK Marks. Available at: https://www.inckmarks.org/docs/new/WhyKidsandWhyCHWs.pdf.
- Bruner, C., D. Willis, C. D. Bethell, P. Dworkin, and K. Johnson. 2021. Medicaid, managed care, and value-based payment systems: state roles in contracting for healthy child development. Child Health Care Transformation Series Working Paper Series No. 8, InCK Marks Initiative. Available at: https://www.inckmarks.org/docs/newresources/Oct2021/WP8ValueBasedMedicaidforChildren.pdf.
- Bruno, E. P., and I. U. Iruka. 2022. Reexamining the Carolina abecedarian project using an antiracist perspective: implications for early care and education research. Early Childhood Research Quarterly 58:165-176. https://doi.org/10.1016/j.ecresq.2021.09.001.
- Bucci, M., L. Gutiérrez Wang, K. Koita, S. Purewal, S. Silvério Marques, and N. Burke Harris. 2015. Center for youth wellness ACE-questionnaire user guide. Available at: https://www.nursing.umaryland.edu/media/son/academics/professional-education/religion-and-ethics/CYW-ACE-Q-USer-Guide-copy.pdf (accessed November 11, 2024).
- Buchanan, G., E. Sullivan, C. Berkel, S. Breitenstein, E. Feinberg, T. Valado, and D. Willis. 2023. Implementing parenting programs in primary care: a framework and a call for action. Academic Pediatrics 23(7):1315-1325. https://doi.org/10.1016/j.acap.2023.04.006.
- Butler, J., L. Gregg, L., R. Calam, and A. Wittkowski. 2020. Parents’ perceptions and experiences of parenting programmes: a systematic review and metasynthesis of the qualitative literature. Clinical Child and Family Psychology Review 23(2):176-204. https://doi.org/10.1007/s10567-019-00307-y.
- Cannon, J., M. Kilburn, L. Karaoly, T. Mattox, A. Muchow, and Buenaventura. 2017. Investing early: taking stock of outcomes and economic returns from early childhood programs. Santa Monica, CA: RAND Corporation. https://doi.org/10.7249/RR1993.
- Carman, K. L., P. Dardess, M. Maurer, S. Sofaer, K. Adams, C. Bechtel, and J. Sweeney. 2013. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Affairs 32(2):223-231.
- Carson, M. C., Z. Montaño, A. R. Kelman, D. M. Coffey, and J. R. Javier. 2019. Promoting behavioral health equity through implementation of the Incredible Years within primary care. Translational Issues in Psychological Science 5(4):390-401. https://doi.org/10.1037/tps0000212.
- CCSP (Center for the Study of Social Policy). 2019. DULCE: A Review of Impact and Insights. Washington, DC: Center for the Study of Social Policy. Available at: https://cssp.org/resource/dulce-review-impact-insights/ (accessed November 11, 2024).
- CSSP and Nurture Connection. 2024. Early Relational Health Supports Families. Available at: https://nurtureconnection.org/family-partnership/ (accessed November 11, 2024).
- CDC (Centers for Disease Control and Prevention). 2020. QuickStats: percentage of children aged <18 years who received a well-child checkup in the past 12 months, by age group and year — national health interview survey, United States, 2008 and 2018. Morbidity and Mortality Weekly Report 69(8):222. https://doi.org/10.15585/mmwr.mm6908a5.
- CDC. 2024. Resources for Community Health Workers. Available at: https://www.cdc.gov/chronic-disease/php/community-health-worker-resources/index.html (accessed May 28, 2024).
- Coker, T. R., S. Chacon, M. N. Elliott, Y. Bruno, T. Chavis, C. Biely, and P. J. Chung. 2016. A parent coach model for well-child care among low-income children: a randomized controlled trial. Pediatrics 137(3):e20153013. https://doi.org/ 10.1542/peds.2015-3013.
- Coker, T. R., P. J. Chung, B. O. Cowgill, L. Chen, and M. A. Rodriguez. 2009. Low-income parents’ views on the redesign of well-child care. Pediatrics 124(1):194-204. https://doi.org/10.1542/peds.2008-2608.
- Committee on Practice and Ambulatory Medicine, Bright Future Periodicity Schedule Workgroup. 2023. 2023 recommendations for preventive pediatric health care. Pediatrics 151(4): e2023061451. https://doi.org/10.1542/peds.2023-061451.
- Community-Based Workforce Alliance. 2021. A Guide to Community-Based Workforce Principles for Pandemic Response and Resilience. Available at: https://healthbegins.org/community-based-workforce-principles/ (accessed November 11, 2024).
- Corôa, R. D. C., A. Gogovor, A. Ben Charif, A. B. Hassine, H. T. V. Zomahoun, R. K. D. McLean, A. Milat, K. V. Plourde, N. Rheault, L. Wolfenden, and F. Legare. 2023. Evidence on scaling in health and social care: an umbrella review. The Milbank Quarterly 101(3):881-921. https://doi.org/10.1111/1468-0009.12649.
- Council on Early Childhood, P. C. High, and P. Klass. 2014. Literacy promotion: an essential component of primary care pediatric practice. Pediatrics 134(2):404-409. https://doi.org/10.1542/peds.2014-1384.
- Council on Children with Disabilities, Medical Home Implementation Project Advisory Committee, R. M. Turchi, R. C. Antonelli, K. W. Norwood, R. C. Adams, T. J. Brei, R. T. Burke, B. E. Davis, S. L. Friedman, A. J. Houtrow, D. Z. Kuo, S. E. Levy, S. E. Wiley, M. A. Kalichman, N. A. Murphy, W. C. Cooley, J. Jeung, B. Johnson, T. S. Klitzner, J. L. Lail, L. L. Lindeke, A. Mullins, L. Partridge, W. Schwab, C. Stille, D. Waldron, N. Wells, and C. Sia. 2014. Patient- and family-centered care coordination: a framework for integrating care for children and youth across multiple systems. Pediatrics 133(5):e1451-e1460. https://doi.org/10.1542/peds.2014-0318.
- Crane, M. E., P. C. Kendall, B. F. Chorpita, M. R. Sanders, A. R. Miller, C. Webster-Stratton, J. Mc William, J. S. Beck, C. Ashen. D. D. Embry, J. A. Pickering, and E. L. Daleiden. 2023. The role of implementation organizations in scaling evidence-based psychosocial interventions. Implementation Science 18(1):24. https://doi.org/10.1186/s13012-023-01280-5.
- Dimovitz, C., S. Butler, K. Wang, K. O’Rourke, S. Cornea, and T. E. Wasser. 2023. Implementing Centering Parenting Model with an urban pediatric population to measure and improve clinical outcomes and parent satisfaction. Journal of Pediatric Health Care 37(3), 221–226. https://doi.org/10.1016/j.pedhc.2022.09.012.
- Doyle, S., S. Chavez, S. Cohen, and S. Morrison. 2019. Fostering social and emotional health through pediatric primary care: common threads to transform everyday practice and systems. Available at: https://cssp.org/wp-content/uploads/2019/10/Fostering-Social-Emotional-Health-Full-Report.pdf (accessed November 11, 2024).
- Dumitriu, D., A. Lavallée, J. L. Riggs, C. A. Frosch, T. V. Barker, D. L. Best, B. Blasingame, J. Bushar, D. Charlot-Swilley, E. Erickson, M. A. Finkel, B. Fortune, L. Gillen, M. Martinez, U. Ramachandran, L. M. Sanders. D. W. Willis, and N. Shearman. 2023. Advancing early relational health: a collaborative exploration of a research agenda. Frontiers in Pediatrics 11:1259022. https://doi.org/10.3389/fped.2023.1259022.
- Dunst, C. J. 2021. Meta-analysis of the relationships between the adequacy of family resources and personal, family, and child well-being. Journal of Psychology and Behavioral Science 9(1). https://doi.org/10.15640/jpbs.v9n1a5.
- Eckenrode, J., M. I. Campa, P. A. Morris, C. R. Henderson Jr, K. E. Bolger, H. Kitzman, and D. L. Olds. 2017. The prevention of child maltreatment through the nurse family partnership program: mediating effects in a long-term follow-up study. Child maltreatment 22(2):92-99.
- Einhorn Family Charitable Trust, Ariadne Labs, and National Institute for Child Health Quality. 2016. Promoting young children’s (0-3) socioemotional development in primary care. Available at: https://nichq.org/sites/default/files/resource-file/Promoting%20Young%20Children%27s%20Socioemotional%20Development%20in%20Primary%20Care%20%282016%29.pdf (accessed April 27, 2024).
- Emery Tavernier R. L., M. Oo, S. Anderson-Badbade, L. Grzejszczak, and P. Rogers. 2024. Prescription for Play research report: a multi-site case study of the process and outcome measures of Prescription for Play. Available at: https://www.weitzmaninstitute.org/wp-content/uploads/2024/04/2023_Full-P4P-Report-for-WI_FINAL-for-Upload.pdf (accessed July 1, 2024).
- Fehr, K. K., B. C. Leraas, and M. M. Littles. 2020. Behavioral health needs, barriers, and parent preferences in rural pediatric primary care. Journal of Pediatric Psychology 45(8):910-920.
- Fisher, P. A., T. V. Barker, and K. N. Blaisdell. 2020. A glass half full and half empty: the state of the science in early childhood prevention and intervention research. Annual Review of Developmental Psychology 2:269-294. https://doi.org/10.1146/annurev-devpsych-121318-084958.
- Ford, C. A., C. Cheek, J. Culhane, J. Fishman, L. Mathew, E. C. Salek, and J. Jaccard. 2016. Parent and adolescent interest in receiving adolescent health communication information from primary care clinicians. Journal of Adolescent Health 59(2):154-161.
- Garbe, C. M., S. L. Bond, C. Boulware, C. Merrifield, T. Ramos-Hardy, M. Dunlap, A. Caldwell, N. Shearman, and A. Miller-Fitzwater. 2023. The effect of exposure to reach out and read on shared reading behaviors. Academic Pediatrics 23(8):1598-1604. https://doi.org/10.1016/j.acap.2023.06.030.
- Garfield, C., and S. Kangovi. 2019. Integrating Community health workers into health care teams without coopting them. Health Affairs Blog, May 10. https://doi.org/10.1377/forefront.20190507.746358.
- Ghandour, R. M., A. H. Hirai, K. A Moore, K. Paschall, D. R. LaForett, E. Reddington, and M. D. Kogan. 2024. School readiness among United States children: results from the 2022 national survey of children’s health. Academic Pediatrics 24(7):1049-1061. https://doi.org/10.1016/j.acap.2024.02.013.
- Gonzalez, C., A. Morawska, and D. M. Haslam. 2018. Enhancing initial parental engagement in interventions for parents of young children: a systematic review of experimental studies. Clinical Child and Family Psychology Review 21:415-432.
- Green, L. W., and M. W. Kreuter. 2005. Health program planning: an educational and ecological approach, 4th ed. New York: McGraw-Hill Education.
- Greenberg, M. R. 2006. The diffusion of public health innovations. American Journal of Public Health 96(2):209-210. https://doi.org/10.2105/AJPH.2005.078360.
- Guastaferro, K., B. S. Lai, K. Miller, J. R. Shanley Chatham, D. J. Whitaker, S. Self-Brown, A. Kemner, and J. R. Lutzker. 2018. Braiding of two evidence-based programs for families at-risk: results of a cluster randomized trial. Journal of Child and Family Studies 27:535-546.
- Guastaferro, K., and J. R. Lutzker. 2019. A methodological review of safecare®. Journal of Child and Family Studies 28(12) 3268–3285. https://doi.org/10.1007/s10826-019-01531-4.
- Hagan, J. F., J. S. Shaw, and P. M. Duncan. 2017. Bright futures: guidelines for health supervision of infants, children, and adolescents, 4th ed. Elk Grove Village, IL: Bright Futures/American Academy of Pediatrics.
- Hammond, B., A. W. Pressman, C. Quinn, M. Benjamin, H. B. Luesse, and L. Mogilner. 2022. Evaluating the keystones of development – an online curriculum for residents to promote positive parenting in primary care. Academic Pediatrics 22(1):151-159. https://doi.org/10.1016/j.acap.2021.06.005.
- Health Resources & Services Administration. 2024. Maternal, Infant, and Early Childhood Home Visiting (MIECHV) Program. Available at: https://mchb.hrsa.gov/programs-impact/programs/home-visiting/maternal-infant-early-childhood-home-visiting-miechv-program (accessed November 11, 2024).
- High, P. C., and P. Klass. 2014. Literacy promotion: an essential component of primary care pediatric practice. Pediatrics 134(2):404-409. https://doi.org/10.1542/peds.2014-1384.
- Hiratsuka, V. Y., M. E. Parker, J. Sanchez, R. Riley, D. Heath, J. C. Chomo, M. Beltangady, and M. Sarche. 2018. Cultural adaptations of evidence-based homevisitation models in tribal communities. Infant Mental Health Journal: Infancy and Early Childhood 39(3):265-275. https://doi.org/10.1002/imhj.21708.
- Hughes, M., A. Joslyn, M. Wojton, M. OʼReilly, and P. Dworkin. 2016. Connecting vulnerable children and families to community-based programs strengthens parents’ perceptions of protective factors. Infants & Young Children 29:116-129. https://doi.org/10.1097/IYC.0000000000000059
- InCK Marks. 2024. Exemplary and evidenced-based healthy parenting in primary care programs, practices, and systems change initiatives: decription and summary from the NASEM Healthy Parenting in Primary Care scoping review. Available at: https://www.inckmarks.org/docs/7-15-2024/INCK%20MARKS%20DESCRIPTIONS%20AND%20SUMMARY%20FOR%20NASEM%20SCOPING%20REVIEW.pdf (accessed November 11, 2024).
- InCK Marks and National Advisory Team of the Integrated Care for Kids. 2021. Transmittal letter to President Biden and Vice-President Harris. Available at: https://img1.wsimg.com/blobby/go/35bcb6ed-a93b-41a3-9ad9-273bceb67f08/downloads/TRANSMITTA%20LETTERWITHSIGNATURESFeb2021.pdf?ver=1713289039821 (accessed November 11, 2024).
- Israel, B. A., E. Eng, A. J. Schulz, and E. A. Parker. 2012. Methods for community-based participatory research for health, 2nd edition. Hoboken, NJ: Jossey-Bass.
- Javier, J. 2023. Positive parenting: the Filipino family health initiative. PowerPoint presentation, Highlands Council PTA webinar (virtual), January 24, 2023.
- Javier, J. R., W. Aguiling, P. Cunanan, A. Sepulveda, D. M. Coffey, J. Castro, L. A. Palinkas, M. D. Kipke, and W. J. Mack. 2023. Short-term outcomes from a pilot randomized controlled trial evaluating a virtual culturally adapted parenting intervention among Filipino parents of school-age children. Cultural Diversity and Ethnic Minority Psychology, ahead of print, October 19. https://doi.org/10.1037/cdp0000616.
- Jimenez, M. E., N. Uthirasamy, J. R. Hemler, A. Bator, K. Malke, D. Lima, P. O. Strickland, U. Ramachandran, B. F. Crabtree, S. V. Hudson, T. I Mackie, and A. L. Mendelsohn. 2023. Maximizing the impact of reach out and read literacy promotion: anticipatory guidance and modeling. Pediatric Research. https://doi.org/10.1038/s41390-023-02945-z.
- Johnson, K., and C. Bruner. 2018. A sourcebook on Medicaid’s role in early childhood: advancing high performing medical homes and improving lifelong health. Des Moines, IA: Child and Family Policy Center. Available at: https://www.inckmarks.org/docs/pdfs_for_Medicaid_and_EPSDT_page/SourcebookMEDICAIDYOUNGCHILDRENALL.pdf.
- Jordan, N., A. K. Graham, C. Berkel, and J. D. Smith. 2019. Costs of preparing to implement a family-based intervention to prevent pediatric obesity in primary care: a budget impact analysis. Prevention Science 20(5):655-664. https://doi.org/10.1007/s11121-018-0970-x.
- Kinney, J. 1994. Beyond the buzzwords: key principles in effective frontline practice. Falls Church, VA: National Center for Service Integration.
- Lasker, R. D., and E. S. Weiss. 2003. Broadening participation in community problem solving: A multidisciplinary model to support collaborative practice and research. Journal of Urban Health: Bulletin of the New York Academy of Medicine 80(1):14-60. https://doi.org/10.1093/jurban/jtg014.
- Lau, R., F. Stevenson, B. N. Ong, K. Dziedzic, S. Treweek, S. Eldridge, H. Everitt, A. Kennedy, N. Qureshi, A. Rogers, R. Peacock, and E. Murray. 2015. Achieving change in primary care—causes of the evidence to practice gap: systematic reviews of reviews. Implementation Science 11(40). https://doi.org/10.1186/s13012-016-0396-4.
- LeCroy, C. W., and D. Lopez. 2020. A randomized controlled trial of healthy families: 6-month and 1-year follow-up. Prevention Science 21(1):25-35.
- Lee, A., J. Ruhter, C. Peters, N. De Lew, and B. D. Sommers. 2023. Medicaid enrollees who are employed: implications for unwinding the Medicaid continuous enrollment provision. Available at: https://www.ncbi.nlm.nih.gov/books/NBK604394/ (accessed November 11, 2024).
- Leslie, L. K., C. J. Mehus, J. D. Hawkins, T. Boat, M. A. McCabe, S. Barkin, E. C. Perrin, C. W. Metzler, G. Prado, V. F. Tait, R. Brown, and W. Beardslee. 2016. Primary health care. American Journal of Preventive Medicine 51(4):S106-S118. https://doi.org/10.1016/j.amepre.2016.05.014.
- Li, J., and T. Ramirez. 2023. Early relational health: a review of research, principles, and perspectives. The Burke Foundation. Available at: https://www.gse.harvard.edu/sites/default/files/2023-09/ERH-Report_final.pdf (accessed November 11, 2024).
- Lloyd, J., K. Moses, and R. Davis. 2020. Recognizing and sustaining the value of community health workers and promotores. Available at: https://www.chcs.org/media/CHCS-CHCF-CHWP-Brief_010920_FINAL.pdf (accessed November 11, 2024).
- Loper, A, B. Woo, and A. Metz. Equity is fundamental to implementation science. Stanford Social Innovation Review 19(3):A3-A5. https://doi.org/10.48558/qngv-kg05.
- Martin, A., A. Waksal, L. Lipton, J. Forman, C. Quinn, M. Benjamin, and B. Hammond. 2020. Educating pediatric residents about parenting: a survey of residency program leaders. Clinical Pediatrics 59(7):699-705. https://doi.org/10.1177/0009922820908584
- Martinez, O., J. Boles, M. Muñoz-Laboy, E. C. Levine, C. Ayamele, R. Eisenberg, J. Manusov, and J. Draine. 2017. Bridging health disparity gaps through the use of medical legal partnerships in patient care: a systematic review. The Journal of Law, Medicine & Ethics 45(2):260-273. https://doi.org/10.1177/1073110517720654.
- Matson, P. A., T. Ridenour, N. Ialongo, R. Spoth, G. Prado, C. J. Hammond, J. D. Hawkins, and H. Adger. 2022. State of the art in substance use prevention and early intervention: applications to pediatric primary care settings. Prevention Science 23(2):204-211. 0.1007/s11121-021-01299-4.
- McCord, M., A. Fierman, S. Sisco, C. Canfield, S. Manjunath, N. Cohen, J. Havens, W. Wilcox, S. Tomopoulos, M. S. Albert, T. Abraham, A. Charney, M. Acri, and K. Piwnica-Worms. 2024. A two-generation, early childhood advanced primary care model. Pediatrics 153(4):e2023062567. https://doi.org/10.1542/peds.2023-062567.
- Mehus, C. J., G. Buchanan, J. Ballard, C. Berkel, I. W. Borowsky, Y. Estrada, J. D. Klein, M. Kuklinski, G. Prado, D. Shaw, and J.D. Smith. 2024. Multiple perspectives on motivating parents in pediatric primary care to initiate participation in parenting programs. Academic Pediatrics 24(3):469-476. https://doi.org/10.1016/j.acap.2023.07.020.
- Mehus, C. J., V. Kazlauskaite, S. Colianni, and I. W. Borowsky. 2019. Parents’ interest in resources to address their child’s behavioral health through primary care. Families, Systems, & Health 37(3):244.
- Miller, M., M. Passarelli, S. Zucker, W. Ake, K. Martini-Carvell, and P. Dworkin. 2023. Help me grow: a model of targeted universalism to advance equity and promote the well-being of all children. Social Innovations Journal 20(2023). Available at: https://socialinnovationsjournal.com/index.php/sij/article/view/6595.
- Mimila, N. A., P. J. Chung, M. N. Elliott, C. D. Bethell, S. Chacon, C. Biely, and T. R. Coker, T. R. 2017. Well-child care redesign: a mixed methods analysis of parent experiences in the PARENT trial. Academic Pediatrics 17(7):747-754.
- Minkler, M., and N. Wallerstein, eds. 2011. Community-based participatory research for health: from process to outcomes. Hoboken, NJ: John Wiley & Sons.
- Moon, D. J., C. B. Nichols, Y. Zhang, A. Cruce, H. Haran, A. Sgourakis, H. Lee, and M. Johnson-Motoyama. 2024. Engagement measures in maltreatment prevention studies: a scoping review. Trauma, Violence, & Abuse 25(2):1551-1567. https://doi.org/10.1177/15248380231188070.
- NASEM (National Academies of Sciences, Engineering, and Medicine). 2015. Strategies for scaling tested and effective family-focused preventive interventions to promote children’s cognitive, affective, and behavioral health. Washington, DC: The National Academies Press.
- NASEM. 2016. Parenting matters: supporting parents of children ages 0-8. Washington, DC: The National Academies Press.
- NASEM. 2019. Fostering healthy mental, emotional, and behavioral development in children and youth: a national agenda. Washington, DC: The National Academies Press.
- NASEM. 2023. Promoting healthy parenting in primary care: evidence for vulnerable and marginalized populations. Available at: https://www.nationalacademies.org/event/41213_12-2023_promoting-healthy-parenting-in-primary-care-evidence-for-vulnerable-and-marginalized-pediatric-populations (accessed November 14, 2024).
- O’Dell, S. M., H. R. Fisher, V. Schlieder, T. Klinger, R. L. Kininger, M. Cosottile, S. Cummings, and K. DeHart. 2021. Engaging parents and health care stakeholders to inform development of a behavioral intervention technology to promote pediatric behavioral health: mixed methods study. JMIR Pediatrics and Parenting 4(4):e27551. https://doi.org/10.2196/27551.
- Office of the Surgen General. 2024. Parents under pressure: the U.S. surgeon general advisory on the mental health and well-being of parents. Washington, DC: HHS Headquarters. Available at: https://www.hhs.gov/sites/default/files/parents-under-pressure.pdf.
- Oo, M., S. Anderson-Badbade, P. Rogers, L. Grzejszczak, and R. L. Emery Tavernier. 2024. A preliminary study of Prescription for Play on developmental concerns. Clinical Pediatrics 0(0). https://doi.org/10.1177/00099228241258846.
- Patlak, M. 2014. Strategies for scaling effective family-focused preventive interventions to promote children’s cognitive, affective, and behavioral health. Washington: The National Academies Press.
- Perrin, E. C., R. Sheldrick, J. M. McMenamy, B. S. Henson, and A. S. Carter. 2014. Improving parenting skills for families of young children in pediatric settings: a randomized clinical trial. JAMA Pediatrics 168(1):16-24. https://doi.org/10.1001/jamapediatrics.2013.2919
- Piccolo, L. R., E. Roby, C. F. Canfield, A. M. Seery, A. Weisleder, C. B. Cates, L. Tutasig, M. Matalon, A. Custode, L. Rodriguez, and A. L. Mendelsohn. 2023. Supporting responsive parenting in real-world implementation: minimal effective dose of the video interaction project. Pediatric Research 95(5):1295-1300. https://doi-org.ezproxy.med.nyu.edu/10.1038/s41390-023-02916-4. doi:10.1038/s41390-023-02916-4.
- Powell, T. W. 2023. Engaging parents in sexual health promotion: lessons learned from adapting Focus on Youth plus Informed Parents and Children Together (FOY+IMPACT). PowerPoint presentation, National Academies Healthy Parenting in Primary Care Collaborative Quarterly Meeting (virtual), September 29, 2023.
- Rhyne, R. L., and L. J. Fagnan. 2018. Practice-based research network (PBRN) engagement: 20+ years and counting. Journal of the American Board of Family Medicine 31(6):833-839. https://doi.org/10.3122/jabfm.2018.06.180274.
- Riley, A. R., B. L. Walker, A. C. Wilson, T. A. Hall, E. A. Stormshak, and D. J Cohen. 2019. Parents’ consumer preferences for early childhood behavioral intervention in primary care. Journal of Developmental & Behavioral Pediatrics 40(9):669-678. https://doi.org/10.1097/DBP.0000000000000736.
- Riley, A. R., B. L. Walker, K. Ramanujam, W. M. Gaultney, and D. J. Cohen. 2021. A mixed-method investigation of parent perspectives on early childhood behavioral services in primary care. The Journal of Behavioral Health Services & Research 49(2):134–148. https://doi.org/10.1007/s11414-021-09772-2.
- Roby, E., E. B. Miller, D. S. Shaw, P. Morris, A. Gill, D. L. Bogen, J. Rosas, C. F. Canfield, K. A. Hails, H. Wippick, J. Honofroff, C. B. Cates, A. Weisleder, K. A. Chadwick, C. D. Raak, and A. L. Mendelsohn. 2021. Improving parent-child interactions in pediatric health care: a two-site randomized controlled trial. Pediatrics 147(3):e20201799. https://doi.org/10.1542/peds.2020-1799
- Rogers, E. M. 2010. Diffusion of Innovations, 5th ed. New York: The Free Press.
- Scheuer, H., M. R. Kuklinski, S. A. Sterling, R. F. Catalano, A. Beck, J. Braciszewski, J. Boggs, J. D. Hawkins, A. M. Loree, C. Weisner, S. Carey, F. Elsiss, E. Morse, R. Negusse, A. Jessen, A. Kline-Simon, S. Oesterle, C. Quesenberry, O. Sofrygin, and T. Yoon. 2022. Parent-focused prevention of adolescent health risk behavior: study protocol for a multisite cluster-randomized trial implemented in pediatric primary care. Contemporary Clinical Trials 112(January):106621. https://doi.org/10.1016/j.cct.2021.106621.
- Schorr, L. B., D. Both, and C. Copple. 1991. Effective services for young children: report of a workshop. In Effective services for young children: report of a workshop. Washington, DC: National Academies Press. Pp. 31-35. https://doi.org/10.17226/1848.
- Schorr, L. B., and D. Schorr. 1989. Within our reach: breaking the cycles of disadvantage. New York: Anchor Books.
- Sege, R., G. Preer, S. J. Morton, H. Cabral, O. Morakinyo, V. Lee, C. Abreu, E. De Vos, and M. Kaplan-Sanoff. 2015. Medical-Legal strategies to improve infant health care: a randomized trial. Pediatrics 136(1):97-106. https://doi.org/10.1542/peds.2014-2955.
- Sepulveda, A., D. M. Coffey, J. David, H. Lopez, K. Bantol, and J. R. Javier. 2021. Creating a culture of mental health in filipino immigrant communities through community partnerships. In Leading community based changes in the culture of health in the US, edited by S. P. F. Claudia and C.-S. Giselle. Rijeka: IntechOpen. https://doi.org/10.5772/intechopen.98458.
- Shelton, R. C., B. R. Cooper, and S. W. Stirman. 2018. The sustainability of evidence-based interventions and practices in public health and health care. Annual Review of Public Health 39:55-76. https://doi.org/10.1146/annurev-publhealth-040617-014731.
- Small Moments Big Impact. 2024. Video Library. Available at: https://smallmomentsbigimpact.com/videos (accessed November 11, 2024).
- Smith, J. D., C. Berkel, J. Rudo-Stern, Z. Montaño, S. M. St. George, G. Prado, A. M. Mauricio, A. Chiapa, M. M. Bruening, and T. J. Dishion. 2018. The Family Check-Up 4 Health (FCU4Health): applying implementation science frameworks to the process of adapting an evidence-based parenting program for prevention of pediatric obesity and excess weight gain in primary care. Frontiers in Public Health 6(October):293. https://doi.org/10.3389/fpubh.2018.00293.
- Spain, A. K., E. K. Monahan, K. Alvarez, and M. Finno-Velasquez. 2021. Latinx family perspectives on social needs screening and referral during well-child visits. MCN: The American Journal of Maternal/Child Nursing 46(3):143-149. https://doi.org/10.1097/nmc.0000000000000710.
- Squires, J., D. Bricker, and E. Twombly. 2002. The ASQ:SE user’s guide for the ages & stages questionnaires: social-emotional. Baltimore, MD: Brookes Publishing.
- Squires, J., L. Potter, and D. Bricker. 1995. The ASQ user’s guide for the ages & stages questionnaires: a parent-completed, child-monitoring system. Baltimore, MD: Brookes Publishing.
- Tamburro, R., A. Pawluszka, D. Amey, E. Tomanio, R. W. Coleman, M. Suttle, A. Eaton, S. R. Beers, K. A. Van, R. Grosskreuz, T. W. October, M A. DiLiberto, R. Willey, S. Bisping, and E. L. Fink. 2023. The Family Network Collaborative: engaging families in pediatric critical care research. Pediatric Research 93(3):453-456. https://doi.org/10.1038/s41390-022-02048-1.
- Underwood, L., and C. Booker. 2020. Black Maternal Health Momnibus Act of 2020, HR 6142, 116th Congress.
- US Census Bureau. n.d. QuickFacts: United States. Available at: https://www.census.gov/quickfacts/fact/table/US/PST045222#PST045222 (accessed June 5, 2024).
- US Department of Health and Human Services and Office of Disease Prevention and Health Promotion. n.d. Social Determinants of Health – Healthy People 2030. Available at: https://health.gov/healthypeople/priority-areas/social-determinants-health (accessed May 30, 2024).
- Viglione, C., and R. Boynton-Jarrett. 2023. The GROWBABY research network: a framework for advancing health equity through community engaged practice-based research. Maternal and Child Health Journal 27(2):210-217. https://doi.org/10.1007/s10995-022-03564-6.
- Vroom. n.d. Behind the research. Available at: https://www.vroom.org/behind-the-research (accessed November 11, 2024).
- Wakschlag, L. S., M. M. Davis, and J. D. Smith. 2024. A vision for implementing equitable early mental health and resilience support in pediatric primary care: a transdiagnostic, developmental approach. Families, Systems, & Health 4(1):6-17. https://doi.org/10.1037/fsh0000884.
- Wakschlag, L. S., M. Y. Roberts, R. M. Flynn, J. D. Smith, S. Krogh-Jespersen, A. J. Kaat, L. Gray, J. Walkup, B. S. Marino, E. S. Norton, and M. M. Davis. 2019. Future directions for early childhood prevention of mental disorders: a road map to mental health, earlier. Journal of Clinical Child & Adolescent Psychology 48(3):539-554. https://doi.org/10.1080/15374416.2018.1561296.
- Waldman, M., K. Hepworth, J. Johnson, K. Tourek, K. Jones, Y. E. Garcia, L. M. Fritz, A. Siebler, and A. Raikes. 2023. Tracking early child development at the population level: validation of the Kidsights Measurement Tool for children birth to age five years. Preprint, Research Square, July 5. https://doi.org/10.21203/rs.3.rs-3084382/v1.
- Webster-Stratton, C., and K. P. McCoy. 2015. Bringing the incredible years programs to scale. New Directions for Child and Adolescent Development 2015(149):81-95. https://doi.org/10.1002/cad.20115.
- Weitzman Institute. 2024. Project ECHO: Childhood Trauma. Available at: https://www.weitzmaninstitute.org/education/weitzman-echo/childhood-trauma (accessed November 11, 2024).
- Wilkinson, R. G., and M. G. Marmot. 1998. The solid facts: social determinants of health. Copenhagen: World Health Organization Regional Office for Europe.
- Williams, A. A. 2020. The next step in integrated care: universal primary mental health providers. Journal of Clinical Psychology in Medical Settings 27(1):115-126.
- World Health Organization and ExpandNet. 2010. Nine steps for developing a scaling-up strategy. Available at https://iris.who.int/handle/10665/44432 (accessed November 11, 2024).
- Wright, J. L., W. S. Davis, M. M. Joseph, A. M Ellison, N. J. Heard-Garris, T. L. Johnson, and the AAP Board Committee on Equity. 2022. Eliminating race-based medicine. Pediatrics 150(1):e2022057998. https://doi.org/10.1542/peds.2022-057998.
- Zero to Three. 2024. Financing Opportunities to Support Integrated Behavioral Health Promotion and Prevention Services, Healthysteps National Office Policy and Finance Team. Available at: https://www.healthysteps.org/wp-content/uploads/2023/07/Behavioral-Health-Prevention-Reimbursement-Opportunities_FINAL.pdf (accessed April 27, 2024).
- Zimmermann, M., W. O’Donohue, M. Zepeda, and A. Woodley. 2021. Examining caretaker attitudes towards primary prevention of pediatric behavioral health problems in integrated care. The Journal of Behavioral Health Services & Research 48(1):120-132
- Zulu, J. M., and H. B. Perry. 2021. Community health workers at the dawn of a new era. Health Research Policy and Systems 19(S3):130. https://doi.org/10.1186/s12961-021-00761-7.


