The National Academy of Medicine’s NAM Perspectives platform extends the National Academies’ convening and advising functions by providing a venue for leading health, medical, science, and policy experts to reflect on issues and opportunities important to the advancement of health, health care, and biomedical science. NAM Perspectives are individually-authored papers that do not reflect consensus positions of the NAM, the National Academies, or the authors’ organizations. They are not reports of the National Academies.
Below, we are pleased to present the top 10 most read NAM Perspectives papers of 2019. These manuscripts cover a wide array of issues, from clinician burnout and well-being to the social determinants of health. Please enjoy revisiting these NAM Perspectives, and sign up to receive more Perspectives in 2020!
#10. Patient-Centered, Integrated Health Care Quality Measures Could Improve Health Literacy, Language Access, and Cultural Competence
I. Bau, R. A. Logan, C. Dezii, B. Rosof, A. Fernandez, M. Paasche-Orlow, and W. F. Wong
Patient-Centered, Integrated Health Care Quality Measures Could Improve Health Literacy, Language Access, and Cultural Competence recommends the integration of health care quality improvement measures for health literacy, language access, and cultural competence. The paper also notes the importance of patient-centered and equity-based institutional performance assessments or monitoring systems. The authors support the continued use of specific measures such as assessing organizational system responses to health literacy or the actual availability of needed language access services such as qualified interpreters as part of overall efforts to maintain quality and accountability. Read the Perspective.
![]() Tweet this! Health literacy, cultural competence, and language access are all critical factors in delivering high-quality care. The #10 most-read #NAMPerspectives of 2019 examines existing approaches we can utilize to ensure all 3 domains are addressed for all patients: https://doi.org/10.31478/201902a #NAMTop10
Tweet this! Health literacy, cultural competence, and language access are all critical factors in delivering high-quality care. The #10 most-read #NAMPerspectives of 2019 examines existing approaches we can utilize to ensure all 3 domains are addressed for all patients: https://doi.org/10.31478/201902a #NAMTop10
Share the graphic below on social media:

#9. Standardized Screening for Health-Related Social Needs in Clinical Settings: The Accountable Health Communities Screening Tool
A. Billioux, K. Verlander, S. Anthony, and D. Alley
Standardized Screening for Health-Related Social Needs in Clinical Settings: The Accountable Health Communities Screening Tool reviews the Centers for Medicare & Medicaid Services (CMS) Accountable Health Communities Model, tested by the Center for Medicare and Medicaid Innovation, designed to addresses this critical gap between clinical care and community services in the current health care delivery system. With input from a panel of national experts and after review of existing screening instruments, CMS developed a 10-item screening tool to identify patient needs in 5 different domains that can be addressed through community services (housing instability, food insecurity, transportation difficulties, utility assistance needs, and interpersonal safety). Clinicians and their staff can use this short tool across a spectrum of ages, backgrounds, and settings, and it is streamlined enough to be incorporated into busy clinical workflows. Just like with clinical assessment tools, results from this screening tool can be used to inform a patient’s treatment plan as well as make referrals to community services. Read the Perspective.
![]() Tweet this! Identifying the burden of unmet health-related social needs is the 1st step to connecting individuals to resources that can address those needs and improve their health. More in our #9 most-read #NAMPerspectives of 2019: https://doi.org/10.31478/201705b #NAMTop10 #pophealthrt
Tweet this! Identifying the burden of unmet health-related social needs is the 1st step to connecting individuals to resources that can address those needs and improve their health. More in our #9 most-read #NAMPerspectives of 2019: https://doi.org/10.31478/201705b #NAMTop10 #pophealthrt
Share the graphic below on social media:

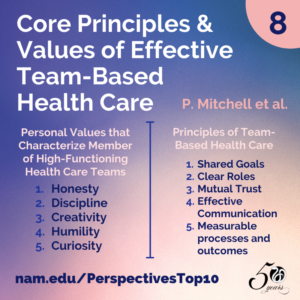
#8. Core Principles & Values of Effective Team-Based Health Care
P. Mitchell, M. Wynia, R. Golden, B. McNellis, S. Okun, C. E. Webb, V. Rohrbach, and I. Von Kohorn
Core Principles & Values of Effective Team-Based Health Care presents basic principles and personal values that characterize interprofessional team-based care. Developed by individual participants from the IOM’s Best Practices Innovation Collaborative, the authors identified key findings from health care literature and used interviews with 11 teams located across the United States to clarify how these factors shape effective team-based care. The principles and values reviewed are intended to help guide clinicians, patients, administrators, and other stakeholders in health care seeking high-value team-based care that focuses on the goals and priorities of patients and their families. In its conclusion, the discussion paper outlines four themes to guide the growth of team-based health care delivery. Read the Perspective.
![]() Tweet this! Physicians caring for Medicare patients may now be connected through one patient to 229 other physicians. @theNAMedicine’s #8 most read #NAMPerspectives outlines values that underpin successful team care: https://doi.org/10.31478/201210c #NAMTop10
Tweet this! Physicians caring for Medicare patients may now be connected through one patient to 229 other physicians. @theNAMedicine’s #8 most read #NAMPerspectives outlines values that underpin successful team care: https://doi.org/10.31478/201210c #NAMTop10
Share the graphic below on social media:
#7. Burnout and Job and Career Satisfaction in the Physician Assistant Profession: A Review of the Literature
A. C. Essary, K. S. Bernard, B. Coplan, R. Dehn, J. G. Forister, N. E. Smith, and V. L. Valentin
While much is known about the prevalence of burnout among physicians and nurses, little is known about burnout in the physician assistant (PA) profession. Approximately 50 percent of physicians and 35 percent of nurses report symptoms of burnout. Burnout is linked to increased health care costs, medical errors, and poor patient outcomes. The PA profession emerged in the 1960s in response to workforce shortages in rural and underserved communities. The profession has evolved from one designed for primary care to one that is adaptable to broad workforce demands. PAs are now employed in almost all medical specialties, including those with physicians reporting high rates of burnout. The authors believe that Burnout and Job and Career Satisfaction in the Physician Assistant Profession: A Review of the Literature is the first paper to explore the literature that relates specifically to PA burnout and career and job satisfaction. Read the Perspective.
![]() Tweet this! Physician assistants are an important part of health care teams, but little research has been done to understand how to best support their well-being & career satisfaction. Read more in our #7 most read #NAMPerspectives of 2019: https://doi.org/10.31478/201812b #NAMTop10 #ClinicianWellBeing
Tweet this! Physician assistants are an important part of health care teams, but little research has been done to understand how to best support their well-being & career satisfaction. Read more in our #7 most read #NAMPerspectives of 2019: https://doi.org/10.31478/201812b #NAMTop10 #ClinicianWellBeing
Share the graphic below on social media:
#6. Gender-Based Differences in Burnout: Issues Faced by Women Physicians
K. Templeton, C. Bernstein, J. Sukhera, L. M. Nora, C. Newman, H. Burstin, C. Guille, L. Lynn, M. L. Schwarze, S. Sen, and N. Busis
Individual, institutional, and societal risk factors for the development of burnout can differ for women and men physicians. While some studies on physician burnout report an increased prevalence among women, this finding may be due to actual differences in prevalence, the assessment tools used, or differences between/among the genders in how burnout manifests. Gender-Based Differences in Burnout: Issues Faced by Women Physicians reviews the prevalence of burnout in women physicians and contributing factors to burnout that are specific for women physicians. Understanding, preventing, and mitigating burnout among all physicians is critical, but such actions are particularly important for the retention of women physicians, given the increasing numbers of women in medicine and in light of the predicted exacerbation of physician shortages. Read the Perspective.
![]() Tweet this! Recognizing gender-related differences in burnout is important for designing successful strategies to improve clinician well-being for everyone. Read more in the #6 most read #NAMPerspectives of 2019: https://doi.org/10.31478/201905a #ClinicianWellBeing
Tweet this! Recognizing gender-related differences in burnout is important for designing successful strategies to improve clinician well-being for everyone. Read more in the #6 most read #NAMPerspectives of 2019: https://doi.org/10.31478/201905a #ClinicianWellBeing
Share the graphic below on social media:
#5. Nurse Suicide: Breaking the Silence
J. Davidson, J. Mendis, A. R. Stuck, G. DeMichele, and S. Zisook
Nurse Suicide: Breaking the Silence aims to raise awareness of and begin to build an open dialogue regarding nurse suicide. Recent exposure to nurse suicide raised our awareness and concern, but it was disarming to find no organization-specific, local, state, or national mechanisms in place to track and report the number or context of nurse suicides in the United States. This paper describes our initial exploration as we attempted to uncover what is known about the prevalence of nurse suicide in the United States. Our goal is to break through the culture of silence regarding suicide among nurses so that realistic and accurate appraisals of risk can be established and preventive measures can be developed. Read the Perspective.
![]() Tweet this! Real-life experiences presented in @theNAMedicine’s #5 most read #NAMPerspectives paper of 2019 aim to shed light on an often under-recognized threat to our health care system: nurse suicide. http://ow.ly/jO9J30hBmqf #NAMTop10
Tweet this! Real-life experiences presented in @theNAMedicine’s #5 most read #NAMPerspectives paper of 2019 aim to shed light on an often under-recognized threat to our health care system: nurse suicide. http://ow.ly/jO9J30hBmqf #NAMTop10
Share the graphic below on social media:
#4. Alternatives to Antibiotics: Why and How
H. K. Allen
Alternatives to Antibiotics: Why and How discusses how the antibiotic resistance problem is caused by the evolution and transfer of genes that confer resistance to medically important antibiotics into human pathogens. The acquisition of such resistance genes by pathogens complicates disease treatment, increases health care costs, and increases morbidity and mortality in humans and animals. As antibiotic resistance continues to evolve, antibiotics of so-called last resort become even more precious. Reducing or preventing the dissemination of antibiotic resistance genes into human pathogens is currently of high international importance. Read the Perspective.
![]() Tweet this! As antibiotic resistance continues to evolve, solutions are more important than ever. @theNAMedicine’s #4 most-read #NAMPerspectives paper of 2019 offers a look at alternatives: http://bit.ly/2uAHzZ7 #NAMTop10
Tweet this! As antibiotic resistance continues to evolve, solutions are more important than ever. @theNAMedicine’s #4 most-read #NAMPerspectives paper of 2019 offers a look at alternatives: http://bit.ly/2uAHzZ7 #NAMTop10
Share the graphic below on social media:
#3. Burnout Among Health Care Professionals: A Call to Explore and Address this Underrecognized Threat to Safe, High-Quality Care
L.N. Dyrbye, T.D. Shanafelt, C.A. Sinsky, P.F. Cipriano, J. Bhatt, A. Ommaya, C.P. West, and D. Meyers
Burnout Among Health Care Professionals: A Call to Explore and Address This Underrecognized Threat to Safe, High-Quality Care discusses how the United States health care system is rapidly changing in an effort to deliver better care, improve health, and lower costs while providing care for an aging population with high rates of chronic disease and co-morbidities. Among the changes affecting clinical practice are new payment and delivery approaches, electronic health records, patient portals, and publicly reported quality metrics—all of which change the landscape of how care is provided, documented, and reimbursed. Navigating these changes are health care professionals (HCPs), whose daily work is critical to the success of health care improvement. Unfortunately, as a result of these changes and resulting added pressures, many HCPs are burned out, a syndrome characterized by a high degree of emotional exhaustion and high depersonalization (i.e., cynicism), and a low sense of personal accomplishment from work. Read the Perspective.
![]() Tweet this! Clinician burnout affects patient safety, productivity, patient satisfaction and health care costs. @theNAMedicine’s #3 most read #NAMPerspectives paper of 2019 examines how further research can help: http://ow.ly/RbnJ30hs1DI #NAMTop10 #ClinicianWellBeing
Tweet this! Clinician burnout affects patient safety, productivity, patient satisfaction and health care costs. @theNAMedicine’s #3 most read #NAMPerspectives paper of 2019 examines how further research can help: http://ow.ly/RbnJ30hs1DI #NAMTop10 #ClinicianWellBeing
Share the graphic below on social media:
#2. Social Determinants of Health 101 for Health Care: Five Plus Five
S. Magnan
As defined by the World Health Organization (WHO), the social determinants of health (SDoH) are “the conditions in which people are born, grow, live, work and age. These circumstances are shaped by the distribution of money, power and resources at global, national and local levels”. The social determinants of health also determine access and quality of medical care—sometimes referred to as medical social determinants of health. Future opportunities may exist in genetics and biological determinants; however, whether modifying these will be as feasible as modifying the social determinants of health is unknown. Social Determinants of Health 101 for Health Care: Five Plus Five considers what we know and what we need to learn about SDoH to achieve the national quality strategy of better care, healthy people/healthy communities, and affordable care. Read the Perspective.
![]() Tweet this! .@theNAMedicine #2 most read #NAMPerspectives paper of 2019 highlights that exploring opportunities to address social determinants of health in health care is imperative for improved patient care. http://ow.ly/aysf30hs11j #NAMTop10 #pophealthRT
Tweet this! .@theNAMedicine #2 most read #NAMPerspectives paper of 2019 highlights that exploring opportunities to address social determinants of health in health care is imperative for improved patient care. http://ow.ly/aysf30hs11j #NAMTop10 #pophealthRT
Share the graphic below on social media:
#1. Implementing Optimal Team-Based Care to Reduce Clinician Burnout
C. D. Smith, C. Balatbat, S. Corbridge, A. L. Dopp, J. Fried, R. Harter, S. Landefeld, C. Martin, F. Opelka, L. Sandy, L. Sato, and C. Sinsky
Team-based health care has been linked to improved patient outcomes and may also be a means to improve clinician well-being. The increasingly fragmented and complex health care landscape adds urgency to the need to foster effective team-based care to improve both the patient and team’s experience of care delivery. Implementing Optimal Team-Based Care to Reduce Clinician Burnout describes key features of successful health care teams, reviews existing evidence that links high-functioning teams to increased clinician well-being, and recommends strategies to overcome key environmental and organizational barriers to optimal team-based care in order to promote clinician and patient well-being. Read the Perspective.
![]() Tweet this! Teamwork has been found to partially mitigate the relationship between work demands and burnout. @theNAMedicine’s #1 most read #NAMPerspectives paper of 2019 details why: https://doi.org/10.31478/201809c #NAMTop10 #ClinicianWellBeing
Tweet this! Teamwork has been found to partially mitigate the relationship between work demands and burnout. @theNAMedicine’s #1 most read #NAMPerspectives paper of 2019 details why: https://doi.org/10.31478/201809c #NAMTop10 #ClinicianWellBeing
Share the graphic below on social media: