
By Jamie Durana
“One of the cultural changes that has to take place is for it to be OK that you’re not OK.”
Kevin Sowers, MSN, RN, FAAN, president of the Johns Hopkins Health System, reflects on a shift that’s gradually reshaping the culture of health care: prioritizing workforce well-being. For years, well-being has been quietly eroding in the background: under-appreciated, under-addressed, and often treated as a personal issue rather than a systemic one. But the toll of burnout, moral distress, and unrelenting pressures is now being recognized as a critical health care challenge that impacts clinicians’ lives and the quality and accessibility of care. Sowers says health care organizations must be committed for the long haul: “One of the hardest things to change is an organization’s culture.”
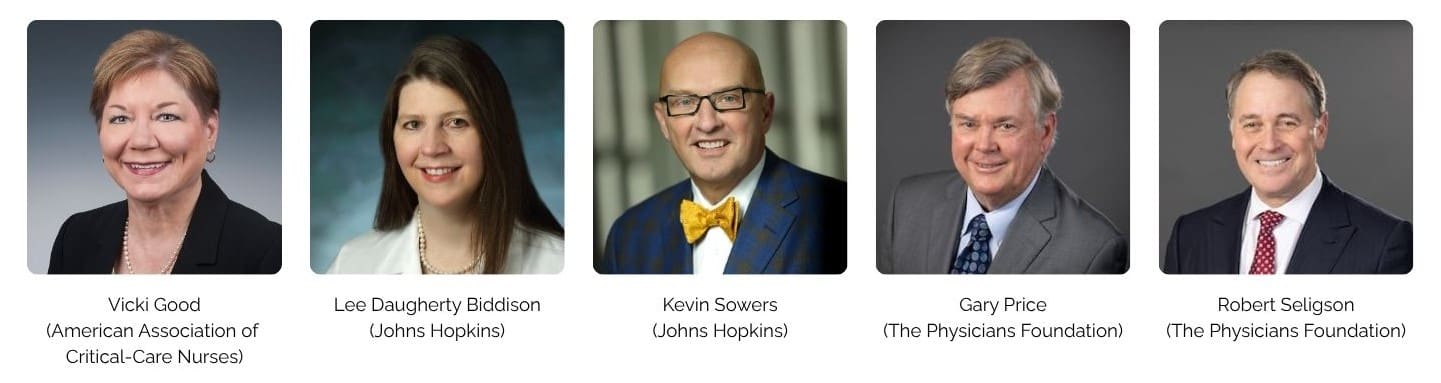
Across the United States and the world, a growing number of health organizations are recognizing that supporting clinician well-being is foundational to a strong health care sector. Since 2017, the National Academy of Medicine’s (NAM) Action Collaborative on Clinician Well-Being and Resilience has been a force behind that shift, convening leaders committed to real change. Three of the Collaborative’s sponsor organizations — the American Association of Critical-Care Nurses, Johns Hopkins Health System, and The Physicians Foundation — are sharing how they’re helping to lead the way.
Why Clinician Well-Being Is an Urgent Priority
The urgency driving these organizations to act didn’t emerge overnight. Although public awareness about health worker burnout grew during the COVID-19 pandemic, leaders from these sponsor organizations explain the burnout crisis had been building for years.
Gary Price, MD, president of The Physicians Foundation, says the pandemic exposed “cracks in the health care system” that demanded policymakers and the public alike pay attention. “The surge in physician distress coupled with persistent stigma around seeking mental health support made it clear that incremental changes were just not enough,” says Price. “The loss of physicians to suicide is estimated to impact 1,000,000 Americans each year — this was a call to action that could not be ignored.”
Robert Seligson, chief executive officer of The Physicians Foundation, shares that his personal physician tragically died by suicide. It was a “wake up call” to the real pressures clinicians and other health workers face, he says. “I’d always put doctors on a pedestal.” Seligson says that finding lasting solutions to a complex problem like the burnout crisis requires collaboration: “Instead of everybody going in 50 different directions, we want to work with a lot of organizations together towards a common goal.”
The Collaborative sponsors are dedicated to building that collective action. Driving a shift in how health worker well-being is viewed and valued is not just about self-care but organizational responsibility and long-term investment in promising initiatives.
The Role of Sponsoring Institutions
While COVID-19 may have brought the workforce crisis into focus, the Collaborative sponsors emphasize awareness is just the first step in a much longer journey.
The mounting data around clinician burnout hits close to home. Price says annual surveys conducted by The Physicians Foundation revealed “alarming data,” and 2024 findings show that more than half of physicians reported frequent feelings of burnout. Sowers has seen this reflected at Johns Hopkins, too: regular surveys revealed burnout among their teams, for both doctors and nurses. “It was a moment where we came together as a leadership team and realized we had to do something different for the health and well-being of our providers,” he says.
For health organizations watching the trends, understanding what meaningful action looks like is not always clear. It’s one thing to acknowledge a workforce crisis; it’s another to know where to begin when addressing problems that have been decades in the making. For the Collaborative’s sponsors, answering that question served as a starting point for sustained commitment.
Rethinking the Work Environment
Vicki Good, DNP, RN, CENP, CPPS, chief clinical officer at the American Association of Critical-Care Nurses (AACN), says the nursing field needs to fundamentally shift its perspective. “Most people go to the hospital to get nursing care,” she explains. “But we’ve ignored the nursing population in relationship to burnout and the work environment.” Good points out that the nursing shortage is expected to grow worse in the next few years, meaning it’s more important than ever for health organizations to make strides in attracting and retaining nursing talent. “Health care is a team sport… we’ve got to have the whole team working together to make it happen,” she says.
However, for any health care worker to be effective, they have to be able to bring their “best self” to their role, Good says. That becomes untenable when the working environment isn’t a healthy one. She emphasizes that well-being initiatives focused on individual resilience won’t go far without ensuring clinicians have a healthy work environment in which to thrive.
Rebuilding Human Connection
Lee Daugherty Biddison, MD, MPH, chief wellness officer at Johns Hopkins, says prioritizing well-being requires addressing the barriers that clinicians face in doing their jobs. People go into the field “really wanting to do the right thing to take care of people and make the world a better place,” but administrative and other strains can get in the way of building positive work environments and connections with patients. Daugherty Biddison emphasizes that supporting effective clinician-patient relationships means supporting everyone: “Any relationship involves two humans, and [the health care sector] just sort of forgot that clinicians were people, too.”
Sowers emphasizes that there’s a direct link between health worker well-being and organizational well-being. He says prioritizing well-being must be treated as “just as important as your performance around quality and safety” because, without that commitment, quality and safety can be negatively impacted. There’s a strong connection between workforce well-being, quality and safety, and patient experience. Sowers says, “the underlying foundation is the well-being of your workforce.”
Building the Evidence Base
Price and Seligson say research and data, like the foundation’s annual surveys, offer critical support for driving systemic change. The organization’s survey findings reveal indicators on the causes of stress and help shed light on strategies for making progress. “We truly get the practicing physicians’ perspective on what’s going on at the ground level to make recommendations,” says Price. Their most recent survey found that the majority of physicians and medical residents reported that administrative burdens — like authorization processes — and the perceived stigma associated with accessing mental health services negatively affected well-being. Seligson says that lessons learned through this research guides the foundation’s approach of sustained investment in understanding the crisis and addressing it through local implementation efforts across the country.
Putting Principles into Action
Good says she’s seeing change in the field: “many organizations have realized the importance of including nurses and other clinicians” in efforts to advance well-being. She says that building a network is critical to driving support for well-being work at health organizations. For AACN, prioritizing networking has helped expand the reach of their work and ensures best practices are shared broadly. Through its work with the Collaborative, AACN is elevating the nursing perspective in discussions on well-being.
Daugherty Biddison emphasizes that “culture change doesn’t happen overnight” and explains that her team works to identify areas where change will have the greatest impact for employees. “We’ve just completed a project that removes the stigmatizing language around seeking mental health support from our credentialing applications,” she says. “That is one of the projects that will impact the entire organization.” Another effort changes the way prior authorizations are handled, embedding pharmacy technicians with clinical care teams. Daugherty Biddison says the result is that everyone can bring their expertise to the process and having an “embedded individual who’s focused specifically on handling [authorizations], with the training to do it, is making a major difference.”
Sowers points to Johns Hopkins’ RISE (Resilience in Stressful Events) Program as an example of culture change in action. The multidisciplinary group of providers is trained to support peers who have experienced a traumatic event at work, and the program connects individuals with ongoing support through the department of psychiatry. Sowers emphasizes that there’s no “one-size-fits-all” approach to well-being and that developing ways to meet different needs is essential.
The Physicians Foundation has focused its grantmaking on systemic change, Seligson says, such as funding initiatives that reduce administrative burdens. He explains that the foundation is also working with medical boards to remove stigmatizing questions about mental health from licensure applications. “There’s a pervasive fear among physicians that seeking mental health care could jeopardize their license or ability to practice,” Price adds. He says that amplifying physicians’ voices has been key: “That helped shift the narrative away from individual resilience and toward systemic change.”
Culture Change Takes Time
The sponsors say culture change is a long game and one worth the effort. One program won’t undo years of dysfunction, but it’s critical that organizations start. Good says it’s hard work, but organizations shouldn’t be deterred from taking a first step. “Realize that … it’s a marathon, it’s not a sprint. You can’t say, ‘OK, we’re going to flip well-being in the next 30 days’ … because you’re changing the culture,” she emphasizes. Good says having a support system, like the Collaborative, to lean on for support is critically important.
Daugherty Biddison echoes the sentiment, saying that having community support provides reassurance that “we’re going to grow together, we’re going to learn together, we’re going to press on together.”

